0836
3D Amide proton transfer weighted imaging in predicting Ki-67 proliferation state of rectal adenocarcinoma1Guangzhou University of Chinese Medicine; The second Affiliated hospital of Guangzhou University of Chinese Medicine;, Guangzhou, China, 2Clinical Science,Philips Healthcare;, Shanghai, China, 3Radiology, The second Affiliated hospital of Guangzhou University of Chinese Medicine, Guangzhou, China
Synopsis
The Accurate preoperative staging and grading are significant on the treatment of protocol selection rectal adenocarcinoma. As a new molecular MR imaging technique, APT imaging could provide information that correlates with tumor cell proliferation. In this study, the capability of APT in differentiating WHO grades and pathologic stages of rectal adenocarcinoma was investigated and compared with DWI. The results show that APT value have a significantly positive correlation with the stage and grade of the rectal adenocarcinoma, and the prognosis factor Ki67.
Purpose and Introduction
Colorectal cancer is the most common gastroenterologic malignancy and rectal adenocarcinoma is a common type of colorectal cancer1. Accurate preoperative assessment of the prognostic factors should be valuable in selecting patients for neoadjuvant therapy and planning surgical approaches to optimize complete excision2. Prognosis in rectal cancer depends strongly on tumor grade and proliferation3. Conventional MR techniques can not detect molecular changes in rectal adenocarcinoma efficiently. APT, using a specific endogeneous material of CEST, semi-quantitatively measure the endogeneous moving proteins and peptide by detecting the reduction in bulk water intensity, which indirectly reflects the changes of the internal environment. In this study, we investigated the capability of APT in differentiating WHO grade and pathologic T and N stages of rectal adenocarcinoma and compared with conventional diffusion weighted imaging (DWI), and to evaluate the correlation between APT and the proliferative factor Ki67.Materials and Methods
Forty-three rectal adenocacinoma patients (average age, 61 years; range, 34–85 years) were scanned on a clinical whole-body 3.0 T MRI system (Ingenia 3.0 T; Philips Health care, Best, the Netherlands). A 32-channel Torso coil was used for signal reception. APT imaging, DWI and Conventional MR sequences (T1-weighted, T2-weighted ) before gadolinium contrast-enhanced imaging (Gd-DTPA; Magnevist; Bayer HealthCare, China) were performed. The three-dimensional APT TSE-mDixon was acquired by quasi-continuous radio frequency (RF) saturation pulse with a duration of 2 seconds. Seven different frequency offsets (±3.5, ±3.42, ±3.58, −1540 ppm) with respect to water frequency (0 ppm) were acquired, and corrected by an inherent B0 field map. The total acquisition time was 4 min 30 s. ADC value were obtained using DWI data with b values of 0 and 1000 sec/mm2. APT images were processed and calculated by the Philips online workstation. Student t test and a one-way analysis of variance were used for statistical analysis. The APTSImean and mean ADC were calculated by averaging signal intensities measured on all slices. Spearman correlation coefficient was calculated between the APTSImean and Ki-67 labeling index (LI) in rectal adenocarcinoma. P < 0.05 was considered to be a statistically significant difference. According to 2007 WHO classification, the tumor is classified as grade 1 (G1, well differentiated) when the volume of gland-like structures occupy greater than 95%, grade 2 (G2, moderately differentiated) greater than 50% but less than or equal to 95%, and grade 3 (G3, poorly differentiated) less than or equal to 50%. Low grade included G1 and G2 tumors, G3 tumors was classified as high grade. Ki-67 LI was defined as the percentage of positive cells among the total number of counted cells and measured by using the standard immunohistochemical staining procedure in all patients.Results
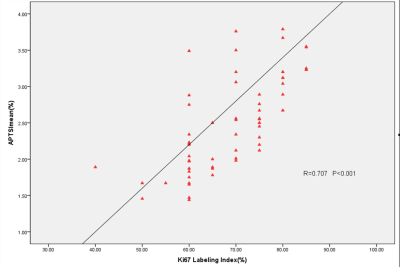
The APTSImean was increased with the advance of TN stage and WHO grade. Concerning to the T stage of rectal adenocarcinoma, the APTSImean of pT4 was significantly higher than those of pT3 and pT2(p<0.05). Other pairwise comparisons did not reveal any significant differences. The APTSImean of the tumors with metastatic lymph nodes (pN1–2) was obviously higher than the tumors without nodal invasion (pN0) (P<.001). In addition, the APTSImean in high-grade tumor were significantly higher than in low-grade ones (P<.001). While significant differences of mean ADC in subgroups of TN stages and WHO grade of rectal adenocarcinoma were not found. The TN stage and WHO grade were significantly positive correlated with the APTSImean (T stage: r=0.712 [95%confidence interval(CI):0.543,0.827, N stage: r=0.348, [95%CI:0.045,0.061], WHO grade: r=0.60, [95%CI:0.371,0.785]), whereas mean ADC showed fair negative correlations with the TN stage and WHO grade (T stage: r=-0.252 [95%CI:-0.504, -0.012], N stage: r=0.208, [95%CI:-0.071, 0.026]). WHO grade: r=0.182, [95%CI:-0.069, 0.393]). The median Ki-67 LI was 70% (range: 40% to 85%). The APTSImean value was positively correlated with Ki-67 LI (r= 0.60, [95%CI: 0.452, 0.8], p< 0.001). With a higher APTSImean indicating greater proliferative activity (Figure2). Figure 1 demonstrate representative images.Conclusion
In conclusion, the APTSImean demonstrated correlations with the TN stage and WHO grades, and performed better than the mean ADC. In addition, APTSImean positively correlated with the Ki-67 proliferation status in this study. 3D TSE APTw MRI would be providing a more comprehensive preoperative assessment of rectal adenocarcinoma patients to benefit therapeutic decision-making in the clinic.Acknowledgements
No acknowledgement found.References
1. Glynne-Jones R, Wyrwicz L, Tiret E, et al. Rectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of oncology: official journal of the European Society for Medical Oncology 2018; 29(Suppl 4): iv263.
2. Y M, S U, A M, et al. Diffusion-weighted magnetic resonance imaging for detecting lymph node metastasis of rectal cancer. 2011; 35(4): 895-9.
3. P K, MJ P, RA L, A S, P R, oncology LCJAjoc. Value of tumor size as a prognostic variable in colorectal cancer: a critical reappraisal. 2011; 34(1): 43-9.
Figures