0816
Cine SSFSE for reduced susceptibility artifact and increased diagnostic accuracy in MR enterography1Department of Radiology, Stanford University, Stanford, CA, United States, 2Global MR applications and Workflow, GE Healthcare, New York, NY, United States
Synopsis
A steady-state free precession (SSFP) sequence is used in many MR enterography (MRE) protocols for acquiring cine images to assess bowel motility, inflammation, and strictures. However, SSFP suffers from susceptibility and banding artifacts that become more significant at high field strengths. In this IRB approved retrospective study, we compared a cine SSFP sequence to a cine T2-weighted single-shot fast spin echo (SSFSE) sequence in 41 patients. We found SSFSE demonstrated significantly superior subjective assessments of image quality, improved diagnostic performance compared to cine SSFP, and successfully mitigated SSFP artifacts that can otherwise limit the exam.
Introduction
MR enterography is an important diagnostic tool in evaluating inflammatory bowel disease (e.g. Crohn’s disease, ulcerative colitis) due to exceptional tissue contrast and lack of ionizing radiation. Currently, a steady-state free precession (SSFP) sequence is used in most clinical practices to acquire a cine loop for assessing bowel motility, inflammation, and strictures. However, SSFP is highly impacted by susceptibility artifacts (mainly due to bowel gas) and banding artifacts, problems that become more severe at higher field-strength (e.g. 3T). In this study, we examine the diagnostic quality of a cine T2-weighted single-shot fast spin echo (SSFSE) sequence intended to supplement or replace SSFP cine sequences in MR enterography.Methods
This IRB approved retrospective study made use of an institutional protocol change to acquire both SSFP and SSFSE based cine sequences on all MR enterography exams. A retrospective cohort of 41 consecutive patients who underwent routine MR enterography were used in this study. Per our standard protocol, patients ingested 450mL of VoLumen (barium sulfate suspension) enteric contrast 90, 60, and 30 minutes before the exam (1350 mL total). The scans included SSFP cine, SSFSE cine, DWI, and pre and post-contrast T1-weighted sequences (Figure 1). The SSFSE sequence used variable refocusing flip angles and outer volume suppression to limit the field of view (Ref. 1 and 2). Due to the time required for T2 signal recovery, each plane of the SSFSE sequence was acquired in an interleaved fashion. These clinical scans were interpreted by radiologists using all the sequences acquired; this clinical interpretation was designated as the gold standard.Two radiologists (10 and 5 years of experience) performed blinded evaluations on the cine SSFP and cine SSFSE sequences in two separate reading sessions at least 1 week apart; which sequence was evaluated first was randomized. Readers assessed for the presence or absence of bowel wall thickening, decreased peristalsis, fistula formation, and stricture formation, in each of three stations: ileum, cecum, and remaining colon, with a confidence rating from 1 to 5, with 5 representing highest confidence. They also rated the subjective quality of the exam from 1 to 5 (with 5 representing highest quality) for bowel motion, small bowel thickening, colonic thickening, the amount of susceptibility artifact in the small and large bowel, as well as overall quality. This protocol thus assessed both objective data on diagnostic accuracy and subjective assessments of image quality.
McNemar’s test was used to assess for statistical significance in the rate of diagnostic errors. Wilcoxon rank-sum test was used to assess for significance in the subjective ratings. Significance was defined as p < 0.05, with a Holm-Bonferroni correction for multiple comparisons.
Results
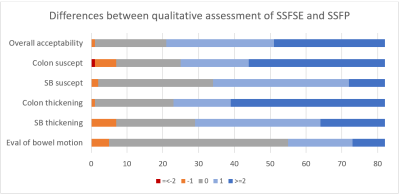
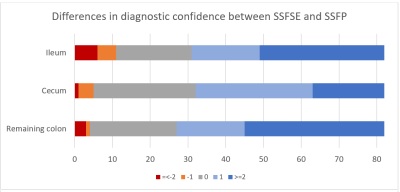
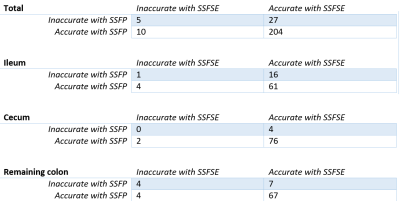
Using the cine SSFSE sequences, raters were significantly more accurate in detecting disease overall (p = 0.0085) and in the ileum (p = 0.0139) (Figure 5). No statistically significant difference was found in diagnostic accuracy in the cecum or remaining colon, although the relatively few cases with disease at those stations limited statistical power. Raters reported significantly greater confidence in their diagnosis with SSFSE at all stations (Figure 4, p<0.00001).Subjectively, raters found SSFSE featured significantly reduced susceptibility artifact, average rating 4.68 for SSFSE vs 3.99 for SSFP in small bowel, 4.15 vs 2.70 in colon (Figure 3, both p < 0.00001). Banding artifacts were eliminated and bowel gas artifacts much reduced with SSFSE, allowing evaluation of the bowel wall in areas (commonly the cecum and descending colon) that were difficult to evaluate with SSFP due to susceptibility artifact.
Raters also significantly favored SSFSE for evaluation of bowel wall thickening (Figure 3, p < 0.00001). For example, in one patient, a fistulous tract was more easily appreciated on SSFSE (figure 2). Scan time was lower for SSFSE compared to SSFP; for example in patient 27 the SSFSE cine required 3.57 minutes, compared to 5.48 minutes for SSFP. Because of the interleaved acquisition protocol, however, temporal resolution is reduced in the SSFSE cine, with an average of 14 seconds between phases compared to 1 second with SSFP. Thus, although the raters found the cine SSFSE superior for evaluation of peristalsis for its clearer delineation of bowel wall (p = 0.00006), its performance in this area may be limited by lower temporal resolution.
Conclusion
Evaluation by expert raters showed overall superior diagnostic performance of SSFSE cine, and significant subjective improvement in image quality and evaluation for disease. Scan time was also reduced, with an average savings of approximately 90 seconds. One limitation of the SSFSE pulse sequence is reduced temporal resolution. Accordingly, cine images feature an apparently random appearance of bowel contraction, compared to the smoother peristaltic appearing movement in the SSFP sequence. Despite this limitation, SSFSE produced both superior diagnostic accuracy and higher subjective ratings for evaluation of peristalsis.As 3T MRI becomes more prevalent, susceptibility artifacts become increasingly problematic occurrences for SSFP sequences in MRE. SSFSE was effective in mitigating susceptibility artifacts, resulting in overall improved diagnostic performance despite the loss of temporal resolution. This sequence therefore merits consideration as a replacement for SSFP cine sequences to benefit from increased SNR at higher field strengths without the limitations of susceptibility artifacts.
Acknowledgements
No acknowledgement found.References
1. J Magn Reson Imaging. 2015 Dec;42(6):1747-58. doi: 10.1002/jmri.24941. Epub 2015 Jun 19. Increased speed and image quality in single-shot fast spin echo imaging via variable refocusing flip angles.
2. Taviani V, Litwiller D, Loening A, Saranathan M, Hargreaves B, Vasanawala S. Single-shot fast spin echo of targeted regions with variable refocusing flip angles and quadratic phase pulses for outer volume suppression. Proc ISMRM, 2015, p. Abstract ID 0948.
Figures
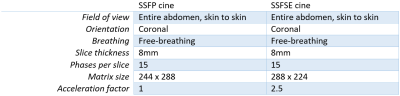
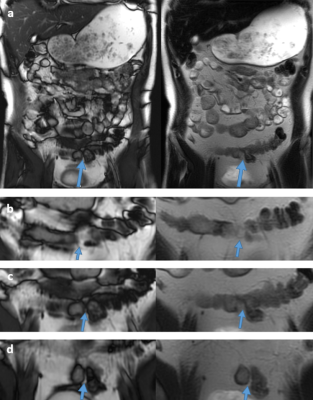
Figure 2a. Still images from SSFP (left) and SSFSE (right) cine sequences of patient 36. The SSFP image is notable for banding artifacts most prominent in the periphery of the image, and for susceptibility artifacts that limit evaluation of the bowel wall. There is a fistulous connection between the distal ileum and sigmoid colon (arrows).
Figure 2b, c, d: Consecutive slices demonstrate greater conspicuity of this fistula (arrows) on the SSFSE sequence.