0650
Cerebrospinal fluid pulse wave velocity measurements using multiband CINE phase-contrast MRI1University of Cologne, Faculty of Medicine and University Hospital Cologne, Institute for Diagnostic and Interventional Radiology, Cologne, Germany, 2University of Cologne, Faculty of Medicine and University Hospital Cologne, Department of General Neurosurgery, Center for Neurosurgery, Cologne, Germany, 3Philips GmbH, Hamburg, Germany
Synopsis
Intraspinal compliance is related to neurological diseases and can be measured by pulse wave velocity (PWV). A multiband CINE phase-contrast MRI sequence was developed to measure the intraspinal PWV between two simultaneously acquired slices along spine. The method was evaluated in-vitro, in healthy-subjects and in a normal pressure hydrocephalus patient. In-vitro results show good reproducibility and dependency on transmural pressure in agreement with theory. A higher PWV compared to healthy subjects is observed in the patient. A decline in PWV after shunt surgery is detected, making it a promising tool for investigation and treatment follow-up of neurological diseases.
Introduction
The compliance describes the ability to accommodate an increase of volume by a specific increase of pressure in a vessel. The intracranial and intraspinal compliance are related to neurological diseases, e.g. normal pressure hydrocephalus (NPH) and Chiari malformation1,2. As the compliance cannot be measured directly, indirect methods were developed. However, these methods are either based on invasive measurements3,4 or multiple non-invasive measurements in combination with complex models using a number of assumptions2,5 An alternative and comparative simple way to indirectly measure compliance and transmural pressure are pulse wave velocity (PWV) measurements in accordance with the Bramwell-Hill equation6. However, high pulse wave velocities and physiological variations (e.g. heart rate) make PWV measurements of the cerebrospinal fluid (CSF) along the spine very challenging. To this end, we developed a new method that enables PWV measurements of the CSF along the spinal cord within one measurement of two simultaneously acquired transversal slices using high temporal resolution multiband CINE phase-contrast MRI (PCMRI) velocity measurements7-9. The new method was evaluated in-vitro, in healthy volunteers and in a normal pressure hydrocephalus patient.Methods
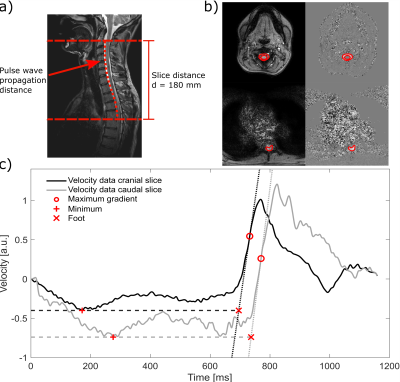
All measurements were carried out on a clinical 3T MRI system (Ingenia, Philips Healthcare, Best, The Netherlands). For PWV measurements two transversal imaging slices were acquired simultaneously using multiband CINE PCMRI with imaging parameters shown in Table 1. To allow for highest temporal resolution as possible only velocity-encoded images were acquired and velocity-compensated acquisition were waived for the PWV measurements. The background phase was removed by subtraction of the first dynamic from all subsequent dynamics. For in-vivo measurements, heart rate was recorded using a wireless pulse oximeter. PWVs were calculated as shown in Figure 1 using a foot-to-foot algorithm10.In-vitro data were acquired using a tube system and a flow pump (CardioFlow 5000, Shelley Medical, London, Ontario, Canada) with 6 different transmural pressure levels, increasing in steps of 5 cmH20, relative to the initial pressure. At each pressure level, the PWV sequence was repeated five times.
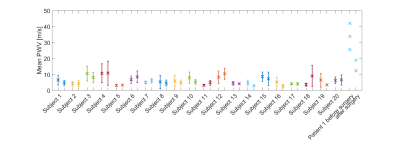
Measurements of PWV in 20 healthy subjects were performed in two subsequent scanning sessions for each subject. In each scanning session, the PWV sequence was repeated five times, resulting in ten measurements per subject.
One 76-year-old male patient suffering from an NPH was included in the study. The patient data were acquired one day before and five days after CSF shunt surgery. The multiband CINE PCMRI sequence was repeated three times in each scan session.
Results
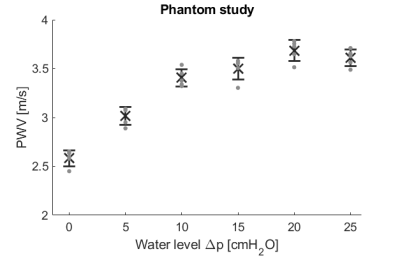
PWVs of the in-vitro study are shown in Figure 2. The minimum and maximum measured PWVs were 2.45 m/s and 3.78 m/s, respectively. The standard deviations for five repeated measurements at the same pressure level reach from 2.36% to 3.24%. Pearson correlation between relative pressure levels and PWV² averaged over repeated measurements was calculated as R = 0.93 (p = 0.008).The mean PWV over all healthy subjects was 5.92 ± 3.81 m/s with. Figure 3 shows the average PWV for each session and subject. The mean absolute difference between average PWVs of session 1 and 2 was 1.53 ± 1.31 m/s, which was found to be not significant using students t-test (p= 0.609).
The mean PWV of the NPH patient measurements before and after surgery were 33.80 ± 6.75 m/s and 15.69 ± 3.37 m/s, respectively (Figure 3).
Discussion
The in-vitro study showed good reproducibility with standard deviations under 5% for repeated measurements. The increasing PWV with increasing pressure seem to follow a square-root-function, in line with the Bramwell-Hill equation6. This is confirmed by the excellent linear correlation between pressure and PWV². The in-vivo data showed no significant differences between the averages of two sessions with 5 repeated PWV measurements. The mean PWV over all subjects is within the range of estimated PWV in previous studies11-13. However, large standard deviations between repeated measurements were found in in-vivo data. As the in-vitro results show smaller standard deviations, these variations may mainly be attributed to physiological variations of the PWV, e.g. due to differences in respiration and heart rate between the repeated measurements, instead of low measurement accuracy. Future studies to investigate the interconnection between physiologic parameters such as heart and respiratory rate and intraspinal compliance and pressure in healthy subjects are warranted.CSF PWV in the NPH patient proved to be markedly higher compared to those in healthy subjects providing evidence for a significantly reduced compliance in NPH. A decrease in PWV was observed after CSF shunt surgery.
Conclusion
A method to measure the PWV of the CSF within one PCMRI measurement was successfully developed and evaluated in-vitro, in healthy-subjects and in an NPH patient. In-vitro results are in good agreement with theory of the Bramwell-Hill equation. In-vivo measurements including the preliminary results in an NPH patient indicated that the presented technique is a very promising tool for investigation, detection, and treatment follow-up of the interconnection between intraspinal compliance and physiological factors or neurological diseases. Further studies will show, if the spinal CSF PWV, which can be assessed rapidly and non-invasively by the presented technique, may be a relevant parameter in the diagnosis of neurological diseases and replace invasive pressure measurements in the future.Acknowledgements
No acknowledgement found.References
1. Bothwell SW, Janigro D, Patabendige A. Cerebrospinal fluid dynamics and intracranial pressure elevation in neurological diseases. Fluids Barriers CNS 2019;16(1):9.
2. Alperin N, Sivaramakrishnan A, Lichtor T. Magnetic resonance imaging-based measurements of cerebrospinal fluid and blood flow as indicators of intracranial compliance in patients with Chiari malformation. Journal of Neurosurgery 2005;103(1):46-52.
3. Marmarou A, Shulman K, LaMorgese J. Compartmental analysis of compliance and outflow resistance of the cerebrospinal fluid system. J Neurosurg 1975;43(5):523-534.
4. Cardoso ER, Rowan JO, Galbraith S. Analysis of the cerebrospinal fluid pulse wave in intracranial pressure. J Neurosurg 1983;59(5):817-821.
5. Alperin NJ, Lee SH, Loth F, Raksin PB, Lichtor T. MR-Intracranial pressure (ICP): a method to measure intracranial elastance and pressure noninvasively by means of MR imaging: baboon and human study. Radiology 2000;217(3):877-885.
6. Bramwell JC, Hill AV. The Velocity of the Pulse Wave in Man. Proceedings of the Royal Society B: Biological Sciences 1922;93(652):298-306.
7. Barth M, Breuer F, Koopmans PJ, Norris DG, Poser BA. Simultaneous multislice (SMS) imaging techniques. Magn Reson Med 2016;75(1):63-81.
8. Breuer FA, Blaimer M, Heidemann RM, et al. Controlled aliasing in parallel imaging results in higher acceleration (CAIPIRINHA) for multi-slice imaging. Magn Reson Med 2005;53(3):684-691.
9. Breuer FA, Blaimer M, Mueller MF, et al. Controlled aliasing in volumetric parallel imaging (2D CAIPIRINHA). Magn Reson Med 2006;55(3):549-556.
10. Latham RD, Westerhof N, Sipkema P, et al. Regional wave travel and reflections along the human aorta: a study with six simultaneous micromanometric pressures. Circulation 1985;72(6):1257-1269.
11. Jackson JR, Williams B. Errors in velocity measurement by the Pitot principle in fluids with slowly propagated pressure waves. J Biomed Eng 1979;1(1):50-54.
12. Kalata W, Martin BA, Oshinski JN, et al. MR measurement of cerebrospinal fluid velocity wave speed in the spinal canal. IEEE Trans Biomed Eng 2009;56(6):1765-1768.
13. Martin BA, Kalata W, Loth F, Royston TJ, Oshinski JN. Syringomyelia hydrodynamics: an in vitro study based on in vivo measurements. J Biomech Eng 2005;127(7):1110-1120.
Figures