0555
Use Environments and Clinical Feasibility of Portable Point-of-Care Bedside Brain MRI
E. Brian Welch1, Samantha By1, Gang Chen1, Hadrien Dyvorne1, Cedric Hugon1, Christopher McNulty1, Anne Nelson1, Rafael O'Halloran1, Michael Poole1, Laura Sacolick1, Nicholas Zwart1, Sean C.L. Deoni2, Joel M. Stein3, Christopher Raio4, Kimon Bekelis5, Gerardo Chiricolo6, Kevin N. Sheth7, and Jonathan M. Rothberg1
1Hyperfine, Guilford, CT, United States, 2Advanced Baby Imaging Lab, Brown University School of Engineering, Providence, RI, United States, 3Department of Radiology, Hospital of the University of Pennsylvania, Philadelphia, PA, United States, 4Emergency Department, Good Samaritan Hospital Medical Center, West Islip, NY, United States, 5Department of Neurological Surgery, Good Samaritan Hospital Medical Center, West Islip, NY, United States, 6Department of Emergency Medicine, New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY, United States, 7Department of Neurology, Yale University School of Medicine, New Haven, CT, United States
1Hyperfine, Guilford, CT, United States, 2Advanced Baby Imaging Lab, Brown University School of Engineering, Providence, RI, United States, 3Department of Radiology, Hospital of the University of Pennsylvania, Philadelphia, PA, United States, 4Emergency Department, Good Samaritan Hospital Medical Center, West Islip, NY, United States, 5Department of Neurological Surgery, Good Samaritan Hospital Medical Center, West Islip, NY, United States, 6Department of Emergency Medicine, New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY, United States, 7Department of Neurology, Yale University School of Medicine, New Haven, CT, United States
Synopsis
Using the world’s first truly portable point-of-care (POC) MRI scanner, it is possible to acquire the fundamental neuro MR imaging contrasts in settings such as the neuro intensive care unit, emergency department, outpatient clinic, and pediatric clinic. Results are presented of neuro MRI exams of children and adults (some with known pathology) using T1W, T2W, FLAIR, and DWI from a low-field portable MRI scanner that transports directly to the patient’s bedside.
INTRODUCTION
Entirely new clinical usage environments are accessible to brain MRI with a scanner that transports directly to the patient’s bedside. Using the world’s first truly portable point-of-care (POC) MRI scanner, it is possible to acquire the fundamental neuro MR imaging contrasts in settings such as the neuro intensive care unit (ICU), emergency department (ED), outpatient clinic, and pediatric clinic. No special room is required, and the scanner is powered by a standard electrical wall outlet. In this abstract, results are presented to evaluate the clinical feasibility of neuro MRI exams of children and adults (some with known pathology) using T1W, T2W, FLAIR, and DWI from a low-field portable POC MRI scanner.METHODS
Under local institutional review board approval, a drivable low-field (64 mT) permanent magnet (Hyperfine, Guilford, Connecticut, USA) was deployed in four different clinical usage environments including a neuro ICU, emergency department, outpatient clinic, and pediatric research clinic (Figure 1). MRI of the brain was acquired on adults and children as young as a 3-month-old. The scanner was fully self-contained with all gradient and RF power amplifiers, spectrometer, and host computer in one chassis. The scanner was plugged into a standard USA 110 Volt, 15 Amp (NEMA 5‑15R) power outlet and controlled via a web-based user interface using a tablet computer. A range of fundamental MR imaging contrasts were acquired as 3D-encoded sequences including magnetization prepared T1-weighted (T1W), T2-weighted (T2W), fluid attenuated inversion recovery (FLAIR), and diffusion-weighted imaging (DWI). Employed data readouts included gradient echo (T1), fast spin echo (T1, T2, FLAIR), and steady-state (DWI) [1]. Figure 2 shows a table of acquisition times, voxel sizes, and other scan parameters for the acquired sequences. After obtaining consent from a patient or guardian, the patient was scanned at the point-of-care. A patient did not leave his/her bed during the MRI exam, and any life monitoring equipment did not need to be removed. Images reconstructed by the scanner were uploaded in enhanced MR DICOM format to the Hyperfine cloud PACS for easy review by key study personnel.RESULTS AND DISCUSSION
To date, more than 200 patients have been successfully imaged by the Hyperfine scanner in neuro ICU, ED, outpatient, and pediatric research settings. Even the most fragile patients, e.g., intubated, wearing a cervical neck collar, or post-craniotomy, were scanned (Figure 3). Observed pathologies included hydrocephalus, hemorrhage, cavernous angioma (Figure 4) as well as ischemic infarct and arachnoid cyst (Figure 5). Despite acquisition outside of an RF-shielded room and in the presence of other equipment, the POC MR images exhibited few artifacts. These promising results indicate the potential positive impact of taking an MRI scanner to locations never thought possible before.CONCLUSION
It is now possible to acquire neuro MRI exams at the point-of-care, i.e., at the patient’s bedside. The ability to image the brain with MRI in heretofore inaccessible clinical usage environments opens up new possibilities to scan the most fragile patients, urgent cases, and youngest children without the need for sedation. In addition to making MRI more widely accessible in the developed world, POC MRI also holds great promise for providing accessible MRI across the globe including developing countries [2]. As evident from other recent developments with low-field MRI systems [3-6], accessible, low-cost scanners are poised to take MRI where it has never gone before.Acknowledgements
This work was supported in part by a collaborative sciences award (17CSA33550004) from the American Heart Association. This work was also supported by research funding from Hyperfine Research, Inc.References
- O’Halloran R, Aksoy M, Van A, Bammer R. 3D isotropic high-resolution diffusion-weighted MRI of the whole brain with a motion-corrected steady-state free precession sequence. MRM 2013; 70(2):466-78.
- Geethanath S. Vaughan J. Accessible Magnetic Resonance Imaging: A Review. JMRI 2019;49:e65-e77.
- McDaniel P, Cooley C, Stockmann J, Wald L. The MR Cap: A single-sided MRI system designed for potential point-of-care limited field-of-view brain imaging. MRM 2019;82:1946-1960.
- Cooley C, Stockman J, Armstrong B, Sarracanie M, Lev M, Rosen M, Wald L. Two-dimensional imaging in a lightweight portable MRI scanner without gradient coils. MRM 2015; 73: 872-883.
- O’Reillly T, Teeuwisse W, Webb A. Three-dimensional MRI in a homogenous 27 cm diameter bore Halbach array magnet. JMR 2019; 307.
- Wald L, McDaniel P, Witzel T, Stockmann J, Cooley C. Low-cost and portable MRI. JMRI 2019. doi: 10.1002/jmri.26942
Figures

Figure 1. The Hyperfine portable
point-of-care MRI scanner (a) deployed at the patient’s bedside in the neuro
intensive care unit (b), emergency department (c), outpatient clinic (d), and pediatric
research clinic (e).
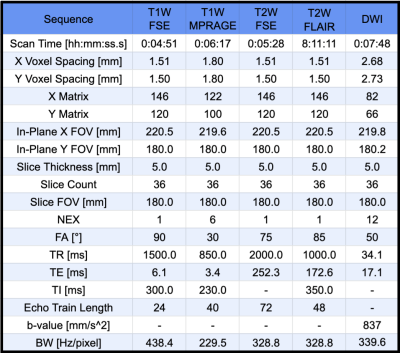
Figure 2. Table of parameters and acquisition details for Hyperfine portable point-of-care MRI sequences.
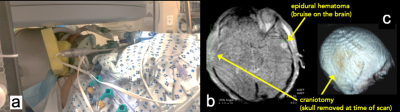
Figure 3.
Examples of fragile patients imaged in the Hyperfine portable point-of-care MRI
scanner including an intubated patient wearing a cervical neck collar (a) and
a
different
sedated motor cycle crash victim with a craniotomy to reduce pressure on the
brain (b, c). A
hematoma (bruise on the brain surface) is observable on the contralateral side
from the site of the impact injury (b). In the 3D surface rendering available
on the Hyperfine user interface, the missing section of skull and the covering
skin flap held in place by staples are clearly visible (c).
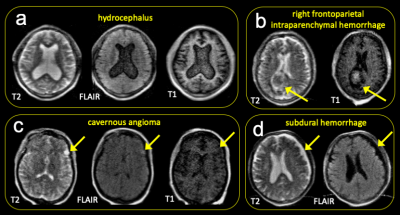
Figure 4.
Example pathologies observed with the Hyperfine portable point-of-care MRI
scanner including hydrocephalus in the outpatient setting (a), right
frontoparietal intraparenchymal hemorrhage in the neuro ICU (b),
cavernous angioma in the outpatient setting (c), and subdural hemorrhage in the neuro
ICU (d).
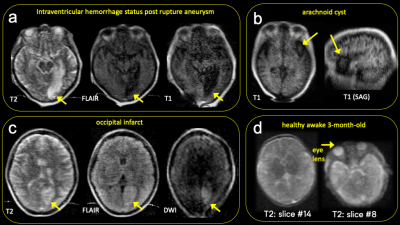
Figure 5.
Example pathologies observed with the Hyperfine portable point-of-care MRI
scanner including an intraventricular hemorrhage status post rupture aneurysm
in the neuro ICU (a), arachnoid cyst in the emergency department (b),
occipital infarct exhibiting DWI (b=837 mm/s2) hyperintensity consistent with restricted diffusion acquired in the neuro ICU setting (c), as
well as a healthy awake 3-month-old in the pediatric research clinic setting (d).