0438
Lung Imaging and Proton Fraction Quantification for Highly Irregular Respiratory Patterns Using Nonuniform Self-Gating1Department of Internal Medicine II, University Ulm Medical Center, Ulm, Germany, 2Core Facility Small Animal Imaging (CF-SANI), Ulm University, Ulm, Germany
Synopsis
Most self-gating methods rely on information that is extracted either from k-space itself or from high temporal resolution sliding-window images. The obtained one-dimensional gating signal is analysed with respect to a dominant and characteristic frequency. These approaches are prone to fail in case of highly non-uniform motion.
The presented application of nonuniform Self-Gating based on a two-dimensional correlation matrix is capable of achieving high resolution proton fraction maps in human subjects with non-regular respiratory motion without the need of time consuming respiratory gating during acquisition.
Introduction
Imaging of lung parenchyma using proton MRI is particularly challenging due to low proton densities in the lung tissue and very short $$$T_2^\star$$$ relaxation times arising from multiple air/water interfaces. While ultrashort echo sequences such as UTE are capable of overcoming $$$T_2^\star$$$ limitations, respiratory compensations are still needed to achieve high resolution images and quantitative information.Self-gating approaches such as DC-based1 or Img-SG2 retrospectively exploit $$$k$$$-space information for respiratory corrections but appear limited in the case of patients with non-regular respiration patterns.
It is shown here, that the concept of nonuniform self-gating (nuSG)3 can achieve quantitative proton fraction maps based on high resolution images also in the case of highly arrhythmic patients. Thereby, nuSG replaces the one-dimensional gating signal of conventional image-based self-gating with a two-dimensional gating matrix, allowing cyclic motion trajectories.
Methods
The nuSG reconstruction is based on 2D UTE lung images (free respiration) with scan parameters shown in table 1. All images were acquired using a tiny golden angle (tyGA) acquisition scheme to minimise motion sensitivity and eddy current artefacts on a 1.5 T whole body MRI system (Achieva 1.5T, Philips Healthcare, Best, The Netherlands) with a dedicated 32-channel cardiac coil. Frames with a temporal resolution of 110 ms (50 spokes) were reconstructed using a sliding window (SW) reconstruction. A region of interest (ROI) is then selected around the lung/liver interface to track respiratory motion over all SW-frames. The correlation matrix is calculated based on the selected ROI according to 3. Each coefficient in the matrix is a measure for the correlation of individual SW-frames with values ranging from zero to one. Each row in the correlation matrix corresponds to a 1D gating signal based on correlation coefficients with respect to the selected row (SW-frame). Afterwards, a correlation tracking algorithm³ is introduced which follows the respiratory motion with respect to the initial SW-frame (first local correlation maximum in first row) along the 2D correlation matrix. Using the Contour Fit, it is possible to combine the k-space data of similar motion states and to reconstruct an associated image with high temporal and high spatial resolution.The capabilities of nuSG compared to a DC-based self-gating approach were tested using two acquisitions, one in which the subject was breathing normally and one in which the subject was instructed to breath highly non-regular. Both gating methods were used to generate an image in the expiratory and inspiratory phase which were then used to calculate the proton fraction $$$f_\text{p}$$$ according to the relation:
$$f_\text{p} = \left( I_\text{lung}/I_\text{muscle} \right)\cdot \exp{T_\text{E}/T_2^\star} \, ,$$ where $$$I_\text{lung}$$$ and $$$I_\text{muscle}$$$ are average signal intensities of the lung and of a reference muscle (chest) respectively. The lung $$$T_2^\star$$$ value of 1.5 ms at 1.5 T was taken from 4.
Results
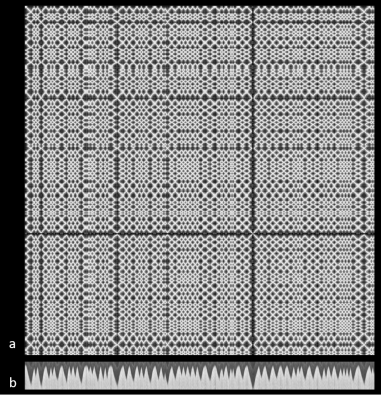
Proton fraction maps for normal and non-regular respiration are shown in figures 1 and 2. While the maps of nuSG and DC-SG reconstructed images are very similar for regular respiratory motion, the lung/liver interface appears significantly blurred in the DC-SG images for the irregular case. The average proton fractions are given in table 2. The proton fractions for normal and non-regular respiration are very similar for nuSG reconstructed images, with deviations under 1 %, comparing equal phases for both respiratory motions (normal and non-regular). For DC-SG images, the proton fractions vary slightly (1.8 %) the exhaled state and strongly (11.9 %) for the inhaled state.In the case of a normal and merely regular respiratory motion, both gating approaches achieve equal image quality with an overall correction of motion artefacts and similar proton fraction values. This is confirmed by the images shown in figure 1 and by the calculated proton fraction values (c.f. table 1). For the case of a highly arrhythmical respiratory motion, the DC-SG approach is not capable of achieving a solid gating signal since bandwidth of respiratory frequencies is significantly increased. Especially in the inspiratory phase, the lung/liver interface appears significantly blurred, leading to unreliable and therefore excluded proton fraction values. As a result, the proton fraction for the inspiratory phase is higher compared to the expiratory phase while the proton fraction values deviate by 11.9 % between normal and arrhythmic respiration. The slight difference for the exhaled state can be explained with Figure 3 (b) - the fully exhaled state always corresponds to a very similar position.
In contrast, the nuSG approach is capable of achieving equal proton fraction values within the same subject (deviations $$$<\,1$$$ %) also in the case of highly arrhythmical respiratory motion.
Discussion and Conclusion
The presented approach is able to handle regular and arrhythmic motion. In the case of regular motion it performs similar to the reference k-space based gating approach. Even in cases of arrhythmic respiration, in which 1D-gating fails, nuSG is able to reconstruct sharp images. With nuSG, the derived proton fraction does not differ significantly between regular and arrhythmic respiration and is in line with the DC-SG values for normal respiration. The nuSG reconstruction is therefore an exciting tool towards the routine use of dynamic lung MRI, as it does not pose any constraints on the breathing pattern of patients.Acknowledgements
The authors thank the Ulm University Centre for Translational Imaging MoMAN for its support.References
[1] Larson A.C., White R.D., Laub G., McVeigh E.R., Li D. and Simonetti O.P. Self-Gated Cardiac Cine MRI. Magn Reson Med. 51, 93-102, 2004.
[2] Tibiletti M., Paul J., Bianchi A., Wundrak S., Rottbauer W., Stiller D. and Rasche V. Multistage three-dimensional UTE lung imaging by image-based self-gating. Magn Reson Med. 75, 1324-1332, 2016.
[3] Wundrak S., Paul J., Radermacher M., Hombach V., Rottbauer W., Bernhardt P. and Rasche V. High-quality reconstruction of arrhythmic cardiac cycles. J Cardiovasc Magn Reson. 18, 2016.
[4] Triphan S.M., Breuer F.A., Gensler D., Kauczor H.U. and Jakob P.M. Oxygenenhanced lung MRI by simultaneous measurement of T1 and T2(*) during freebreathing using ultrashort TE. J Magn Reson Imaging. 41, 1708-1714, 2015
Figures