0437
Which is the Best Method for NSCLC Recurrence Evaluation among MRI, PET/MRI, PET/CT and Standard Examination in Large Prospective Cohort?1Radiology, Fujita Health University School of Medicine, Toyoake, Japan, 2Radiology, Kobe University Graduate School of Medicine, Kobe, Japan, 3Canon Medical Systems Corporation, Otawara, Japan, 4Diagnostic Radiology, Hyogo Cancer Center, Akashi, Japan
Synopsis
Direct comparison of non-small cell lung cancer (NSCLC) recurrence evaluation among these four methods in large prospective cohort more than 400 patients had not been reported. We hypothesize that whole-body MRI as well as PET/MRI had better potential for postoperative NSCLC recurrence than PET/CT and standard radiological examination in large prospective cohort. The purpose of this study was thus to compare the diagnostic performance of whole-body MRI, PET/MRI, PET/CT and standard radiological examination for postoperative NSCLC recurrence assessment in large prospective cohort more than 400 patients.
Introduction
Postoperative recurrence evaluation is important for improving patients’ survival and quality of life in non-small cell lung cancer (NSCLC) patients. For a few decades, detection of recurrent disease using standard radiological examinations such as chest radiograph and/or computed tomography (CT) remained difficult, but positron emission tomography (PET) with [18F] fluoro-2-D-glucose as well as PET combined with CT (PET/CT) have been found to be more effective than standard radiological examination. In addition, it has been suggested that whole-body magnetic resonance imaging (MRI) and PET fused with MRI (PET/MRI) have been suggested as useful for staging and recurrence assessment in NSCLC patients since 2015 (1-3). However, studies directly compared among MRI, PET/MRI, PET/CT or standard examination were tested in less than 100 patients (2, 3). Therefore, no direct comparison of NSCLC recurrence evaluation among these four methods in large prospective cohort more than 400 patients had been reported. We hypothesize that whole-body MRI as well as PET/MRI had better potential for postoperative NSCLC recurrence than PET/CT and standard radiological examination in large prospective cohort. The purpose of this study was thus to compare the diagnostic performance of whole-body MRI, PET/MRI, PET/CT and standard radiological examination for postoperative NSCLC recurrence assessment in large prospective cohort more than 400 patients.Materials and Methods
484 consecutive postoperative NSCLC patients (289 men, 195 women; mean age 69 years) prospectively underwent whole-body MRI at a 3T system (Vantage Titan 3T, Canon Medical Systems Corporation, Otawara, Japan), integrated PET/CTs and standard radiological guideline based on International Association for the Study of Lung Cancer guideline as well as follow-up or pathological examinations. Then, all patients were divided into recurrence (n=42) and non-recurrence (n=442) groups based on pathological and follow-up examinations. All co-registered PET/MRIs were generated by means of our proprietary software. Then, probability postoperative recurrence in each patient was visually assessed on all methods by means of 5-point visual scoring system. To compare diagnostic performance among all methods, receiver operating characteristic analyses were performed. Then, diagnostic accuracy of postoperative recurrence was statistically compared each other by using McNemar’s test. Agreements were considered as poor for κ< 0.21, fair for κ = 0.21–0.40, moderate for κ = 0.41–0.60, substantial for κ = 0.61–0.80, and excellent for κ = 0.81–1.00. A p value < 0.05 was considered statistically significant for all statistical analyses.Results
Representative case is shown in Figure 1 and 2. Interobserver agreements for postoperative recurrence on all methods were substantial (MRI: κ=0.64, p<0.0001; PET/MRI: κ=0.67, p<0.0001; PET/CT: κ=0.68, p<0.0001; standard radiological examination: κ=0.67, p<0.0001). Results of ROC analysis and McNemar’s test are shown in Figure 3. Area under the curve (AUC) of PET/MRI (AUC=0.99, p<0.05) were significantly larger than that of others (MRI: AUC=0.97, PET/CT: AUC=0.97, standard radiological examination: AUC=0.94). Sensitivity (SE), specificity (SP) or accuracy (AC) of PET/MRI (SE: 92.9%, SP: 98.2%, AC: 97.7%) were significantly higher than that of MRI (SE: 76.2%, p<0.05; AC: 96.3%, p<0.05), PET/CT (SP: 95.5%, p<0.05; AC: 94.8%, p<0.05) and standard radiological examination (SP: 90.5%, p<0.05; AC: 90.0%, p<0.05). In addition, SP (98.2%) and AC of MRI were significantly higher than those of PET/CT and standard radiological examination (p<0.05). Moreover, SP and AC of PET/CT were significantly higher than those of standard radiological examination (p<0.05).Conclusion
Whole-body MRI as well as PET/MRI have significantly better potential for postoperative NSCLC recurrence evaluation than PET/CT and standard radiological examination, although PET/MRI can improve diagnostic performance of MRI in large prospective cohort.Acknowledgements
Authors wish to thank Mr. Katsusuke Kyotani and Prof. Takamichi Murakami in Kobe University Hospital for their valuable contributions to this study.References
- Kim HS, Lee KS, Ohno Y, van Beek EJ, Biederer J. J Magn Reson Imaging. 2015; 42(2): 247-260.
- Ohno Y, Koyama H, Yoshikawa T, et al. Radiology. 2015; 275(3): 849-861.
- Ohno Y, Yoshikawa T, Kishida Y, et al. J Magn Reson Imaging. 2017; 46(6): 1707-1717.
Figures
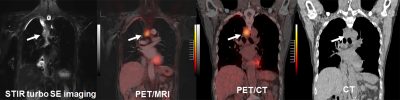
Figure 1. 74-year-old male invasive adenocarcinoma (pT2aN1M0: pStage IIB) patient as having postoperative mediastinal lymph node recurrence.
STIR turbo spin-echo (SE) image, PET/MRI and PET/CT clearly demonstrate mediastinal lymph node recurrence (arrows) and were scored as 5 on all methods, although the recurrence (arrow) is suspected on CT and was scored as 4. This case was true-positive on each method.
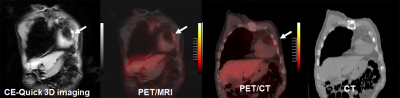
Figure 2. 68-year-old male patient with invasive adenocarcinoma (pT1cN0M0: pStage IA3) patient as having postoperative left rib metastasis.
Contrast-enhanced (CE-) Quick 3D images, PET/MRI and PET/CT demonstrate left rib metastasis (arrows) and were scored as 5 on CE-Quick 3D image and PET/MRI and as 3 on PET/CT, although the recurrence (arrow) is not suspected on CT and was scored as 2. This case was true-positive on MRI and PET/MRI and false-negative on PET/CT and CT as standard radiological examination.
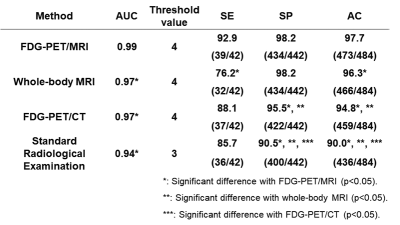
Figure 3. Results of ROC analysis and McNemar’s test.
Area under the curve (AUC) of PET/MRI were significantly larger than that of others (p<0.05). Sensitivity (SE), specificity (SP) or accuracy (AC) of PET/MRI were significantly higher than that of MRI (p<0.05), PET/CT (p<0.05) and standard radiological examination (p<0.05). In addition, SP and AC of MRI were significantly higher than those of PET/CT and standard radiological examination (p<0.05). Moreover, SP and AC of PET/CT were significantly higher than those of standard radiological examination (p<0.05).