0435
Thoracic imaging using balanced steady-state free precession with half-radial dual-echo readout (bSTAR)1Radiological Physics, University of Basel Hospital, Basel, Switzerland, 2Department of Biomedical Engineering, University of Basel, Allschwil, Switzerland
Synopsis
This work demonstrates the application of single-breathold thoracic MRI with balanced steaty-state free precession half-radial dual-echo readout technique (bSTAR) in human subjects. The proposed imaging technique combines a minimal-TR acquisition with a smoothly interleaved Archimedean spiral trajectory, which results in markedly improved signal intensity from low proton lung parenchyma tissue, improved visualization of the pulmonary vascular tree as well as a successful mitigation of eddy current and cardiac motion artifacts.
Introduction
The application of 1H MRI to study lung anatomy and physiology is challenging due to the well-known physical and technical difficulties related to the properties of lung parenchyma. However, imaging techniques such as ultra-short echo time (UTE)1,2 or balanced steady-state free precession (bSSFP)3,4 show promise to overcome the limitations of pulmonary MRI on modern MR-systems.In this work we explore the prospects of a half-radial dual-echo bSSFP pulse sequence termed bSTAR with minimal TR settings for high-resolution large field-of-view acquisitions of chest images during a single breathhold. For the reduction of the eddy currents and motion induced artifacts we implemented a sampling strategy based on a smoothly-interleaved Archimedean spiral trajectory. Furthermore, the results of bSTAR imaging have been compared to the contemporary isotropic SPGR imaging2.
Methods
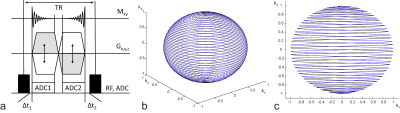
bSTAR imaging3D bSTAR half-radial dual-echo acquisition scheme uses a bSSFP kernel with a non-selective rectangular RF excitation pulse and a bipolar readout gradient as previously proposed by Diwoky et al5. Consequently, the k-space center is sampled with center-out and center-in half-radial projections. The projections are rotated around the center of the k-space and its direction in spherical coordinates follows an Archimedean spiral trajectory6. For the mitigation of eddy-currents, large jumps in the k-space have to be avoided7. Hence, the consecutive spiral interleaves alternate the direction in which they traverse the k-space along the azimuthal axis. Figure 1 shows the bSTAR pulse sequence diagram and the Archimedean spiral trajectory with two interleaves.
MR data acquisition
Experiments were performed on 1.5T MR-scanner (MAGNETOM Avanto-Fit, Siemens Healthineers, Erlangen, Germany). Four healthy volunteers (mean age: 40.2 years, range: 30-52 years, three male, one female) were scanned with a 3D bSTAR and 3D SPGR variant for signal comparison. The study was approved by the Institutional Review Board, and written informed consent was obtained from volunteers prior to the examinations. All scans were performed with predefined shim settings, field-of-view = 45×45×45 cm3, one to thirty-two spiral interleaves and twofold readout oversampling, 24s acquisition time. bSTAR imaging parameters were: TE1/TE2/TR = 0.12/1.18/1.39ms, 17000 radial half-spokes, 320 samples per half-spoke, 200us hard RF pulse, flip angle α = 20°, 2604Hz/pixel bandwidth, 24s acquisition time. The parameters of half-radial SPGR (i.e. UTE acquisition) were as follows: TE/TR = 0.07/3.90 ms, 5870 radial half-spokes, 704 samples per half-spoke, 100us hard RF pulse, flip angle α = 5°, 947Hz/pixel bandwidth.
Image reconstruction
K-space trajectory correction of the radially acquired data was performed using the method proposed by Duyn et al8. Subsequently, bSTAR and SPGR datasets were reconstructed off-line using a gridding algorithm with Kaiser-Bessel kernel9, as well as compressed sensing with a fast iterative shrinkage-thresholding algorithm (FISTA-Mod)10. The datasets were reconstructed on a 3843 matrix resulting in 1.7mm isotroopic resolution, which was interpolated to 1.2mm. The reconstruction pipeline was written in C++ as stand-alone software with CUDA Toolkit 10.1 (NVIDIA Corp. Santa Clara, CA). Datasets were reconstructed in approximately 5 minutes using 20 FISTA-Mod iterations on a workstation equipped with Quadro P6000 GPU (NVIDIA Corp.).
Results
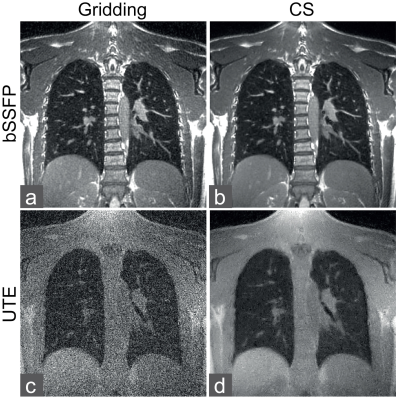
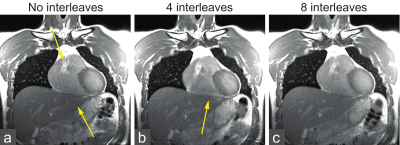
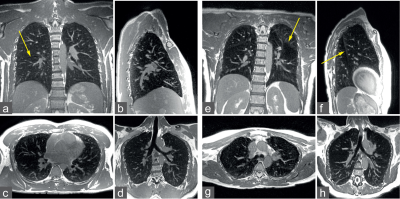
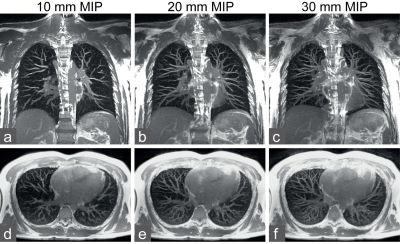
A visual comparison between images reconstructed using gridding and FISTA-Mod from bSTAR and SPGR datasets is shown in Figure 2. Due to the much shorter TR in the bSTAR acquisition it was possible to sample 2.9 more radial half-projections than with the SPGR scan. The ratio between signal magnitude measured in bSTAR and SPGR (ζ = SbSTAR/SSPGR) in the lung parenchyma and blood was 4.2±2.5 and 4.1±0.4, respectively. bSTAR images acquired with one, four and eight spiral interleaved are shown in Figure 3. Coronal, sagittal, axial and oblique views acquired with bSTAR in a single-breathold in two volunteers are shown in Figure 4. Sufficiently high signal intensity in the lung parenchyma enabled us to observe fissures separating the lung lobes, differences between signal intensity in lobes, as well as gravity-related signal intensity differences. Figure 5 shows coronal and axial maximum intensity projection reconstructions for the detailed visualization of the pulmonary vasculature with bSTAR. No noticeable ghosting or banding artifacts can be observed.Discussion and Conclusion
In this work, we explored single-breathold bSTAR thoracic imaging using half-radial dual-echo readouts distributed along smoothly-interleaved Archimedean spiral trajectories. The proposed imaging technique profits from the application of a minimal-TR bSSFP kernel, resulting in markedly improved signal intensity from low proton lung parenchyma tissue. The application of an adapted interleaved spiral trajectory improved the robustness in the presence of cardiac motion, while a very short TR allows for a near complete mitigation of banding artifacts. Future studies will focus on a possible combination of bSTAR with respiratory gating as well as on testing the feasibility in patients with pulmonary disease.Acknowledgements
No acknowledgement found.References
1. Johnson KM, Fain SB, Schiebler ML, Nagle S. Optimized 3D ultrashort echo time pulmonary MRI. Magn Reson Med 2013;70:1241–1250.
2. Wielpütz MO, Triphan SMF, Ohno Y et al. Outracing Lung Signal Decay - Potential of Ultrashort Echo Time MRI. Rofo. 2019 May;191(5):415-423.
3. Bieri O, Markl M, Scheffler K. Analysis and compensation of eddy currents in balanced SSFP. Magn Reson Med. 2005;54:129–137.
4. Heye T, Sommer G, Miedinger D et al. Ultrafast 3D balanced steady-state free precession MRI of the lung: Assessment of anatomic details in comparison to low-dose CT. J Magn Reson Imaging. 2015 Sep;42(3):602-9.
5. Diwoky C, Stollberger R. 3D Radial bUTE. In: Proceedings of the 19th Annual Meeting of ISMRM. Montreal; 2011; p. 387.
6. Wong STS, Roos MS. A strategy for sampling on a sphere applied to 3Dselective RF pulse design. Magn Reson Med 1994;32:778–784.
7. Markl M, Leupold J, Bieri O et al. Double average parallel steady-state free precession imaging: optimized eddy current and transient oscillation compensation. Magn Reson Med. 2005 Oct;54(4):965-74.
8. Duyn JH, Yang Y, Frank JA, van der Veen JW. Simple correction method for k-space trajectory deviations in MRI. J Magn Reson. 1998 May;132(1):150-3.
9. Jackson JI, Meyer CH, Nishimura DG, Macovski A. Selection of a convolution function for Fourier inversion using gridding. IEEE Trans Med Imaging 1991;10:473–478.
10. Iliang J, Schoenlieb CB. Improving “Fast Iterative Shrinkage-Thresholding Algorithm”: Faster, Smarter and Greedier. arXiv preprint:1811.0143, 2018.
Figures