0429
Non-contrast-enhanced 3D-UTE MRI for pulmonary Imaging of Immunocompromised Patients during Hematopoietic Stem Cell Transplantation1Department of Diagnostic and Interventional Radiology, University Hospital Würzburg, Würzburg, Germany, 2Department of Internal Medicine II, University Hospital Würzburg, Würzburg, Germany, 3Application Development, Siemens Healthcare GmbH, Erlangen, Germany
Synopsis
Immunocompromised patients during HSCT procedure commonly need repeated MDCT examinations resulting in a high cumulative radiation dose. 3D-UTE MRI using a stack-of-spirals trajectory, enables contrast-free and radiation-free imaging of the lungs within a single breath-hold with increased signal yield due to echo times being well below parenchymal T2*. 3D-UTE MRI allows diagnostics of inflammatory consolidations and pleural effusions with high sensitivity, specificity and consistency when compared to MDCT. Moreover, 3D-UTE sequences improve detection rates of ground glass opacities in pulmonary MRI.
Introduction
Pneumonia is an important cause of morbidity and mortality in immunocompromised patients with hematopoietic disease especially during hematopoietic stem cell transplantation (HSCT). To date, multidetector computed tomography (MDCT) is the reference technique to assess inflammatory or structural changes to the lung parenchyma in immunocompromised patients1. Repeated MDCT imaging is commonly necessary during HSCT procedure resulting in high cumulative radiation dose2. Due to recent technical advances, radiation-free magnetic resonance imaging (MRI) has become a competitor to MDCT regarding imaging of pulmonary pathologies. Using echo times (TE) of ~0.2 msec - being well below parenchymal T2* - MRI sequences with ultrashort echo time (UTE) allow for significantly increased signal yield. To date, UTE sequences provide whole-chest coverage in 3D and reduced susceptibility to motion artifacts enabling lung MRI in MDCT-like quality3,4. The purpose of this study was to evaluate the feasibility of non-contrast-enhanced 3D-UTE MRI for pulmonary imaging in immunocompromised patients during HSCT procedure.Methods
3D-UTE MR imaging was acquired on a 3T system (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany) using a three-dimensional prototypic UTE Spiral VIBE sequence employing a stack-of-spirals trajectory5, iPAT factor 2, and SPIRiT reconstruction6. Sequence parameters were set as follows: TE = 0.05 ms; TR = 2.35 ms; flip angle = 5°; nonselective hard pulse duration = 60 µs; FOV = 600 mm x 600 mm; resolution = 2.3 x 2.3 x 2.3 mm; number of spiral readouts per partition = 264; number of partitions acquired with 264 spiral arms each = 102 ± 14; reduced slice resolution by 6/8 partial-Fourier imaging; acquisition time < 3 min. Following institutional review board approval, twenty-three patients with an indication for allogeneic HSCT were included into this prospective single-center study and underwent pulmonary MRI before HSCT initiation, in case of CT-proven pneumonia and before discharge following completion of HSCT. MRI was acquired in five different breathing states (deep inspiration, normal inspiration, intermediate breathing state, normal expiration and deep expiration) within a single breath-hold of 12.7-17.6s each. 3D-UTE MR image sets were separately reviewed by two radiologists regarding presence of pleural effusions (PE), ground glass opacities (GGO) and consolidations. MDCT scans acquired within a maximum time interval of three days from MRI were used as reference examinations and assessed regarding the same items in consensus reading.Results
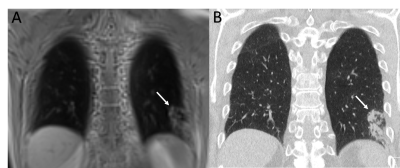
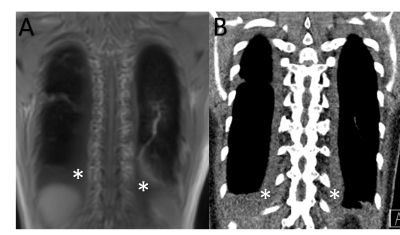
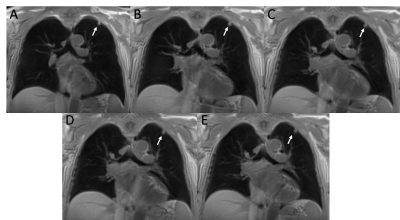
Thirty-three MRI scans were acquired within three days from MDCT acquisition. 3D-UTE MRI allowed for sufficient imaging of pulmonary consolidations (Figure 1) and PE (Figure 2) with high sensitivity (consolidations, 89%; PE, 88%), specificity (consolidations, 87%; PE, 100%) as well as high PPV (consolidations, 88%; PE, 100%) and NPV (consolidations, 84%; PE, 97%). Regarding GGO (sensitivity, 61%; specificity, 86%; PPV, 51%; NPV, 90%), the diagnostic performance of 3D-UTE MRI was distinctly lower. Overall consistency rates between CT and MRI were high (consolidations, 86%; PE, 98%; GGO, 81%). Interrater agreement was good (consolidations, κ = 0.75; PE, κ = 0.83), except for GGO, where the agreement level was moderate (κ = 0.53). None of the acquired five breathing states provided constant superior or inferior detectability regarding the assessed lung pathologies (Figure 3).Discussion
Acquisition times of 3D-UTE MRI and MDCT imaging were similar. 3D-UTE MRI provided sufficient diagnostic imaging of pulmonary consolidations and pleural effusions. Regarding imaging of ground glass opacities, which is especially challenging in pulmonary MRI, the performance of 3D-UTE MRI in our study was superior when compared to results published earlier using a sequence setup of combined T2w HASTE and T1w 3D VIBE (sensitivity 35%)7. Two of twenty-three patients in our study showed exclusive ground glass opacity without any concomitant consolidations. In five other patients, areas of ground glass were accompanied by areas of consolidations, and none of these patients were missed having an inflammatory pulmonary complication during HSCT procedure by both observers. No certain breathing state of 3D-UTE MRI acquisition was found to be superior regarding identification of the assessed pulmonary pathologies. However, image acquisition in inspiratory breath-hold is easier to tolerate for respiratory impaired patients and showed less artifacts from breathing motion.Conclusion
With an acquisition time similar to MDCT, radiation-free and contrast-free 3D-UTE MRI can be expected to play a major role in future pulmonary imaging for example in diagnostics and follow-up of immunocompromised patients with pneumonia.Acknowledgements
The project underlying this report was funded by the Deutsche Forschungsgemeinschaft (DFG).
The Department of Radiology receives a research grant from Siemens Healthcare GmbH. The grant is not specifically directed towards any of the authors.
References
1. Richenberg J, Harvey C. The utility of CT in imaging chest infections in HIV-negative patients. Curr Opin Pulm Med. 1999;5(3):179-84.
2. Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277-84.
3. Wielputz MO, Triphan SMF, Ohno Y, Jobst BJ, Kauczor HU. Outracing Lung Signal Decay - Potential of Ultrashort Echo Time MRI. Rofo. 2019;191(5):415-23.
4. Higano NS, Fleck RJ, Spielberg DR, Walkup LL, Hahn AD, Thomen RP, et al. Quantification of neonatal lung parenchymal density via ultrashort echo time MRI with comparison to CT. J Magn Reson Imaging. 2017;46(4):992-1000.
5. Mugler JP MC, Pfeuffer J, Stemmer A, Kiefer B. Accelerated Stack-of-Spirals Breath-hold UTE Lung Imaging. Proc Intl Soc Mag Reson Med 2017:4904.
6. Lustig M, Pauly JM. SPIRiT: Iterative self-consistent parallel imaging reconstruction from arbitrary k-space. Magn Reson Med. 2010;64(2):457-71.
7. Attenberger UI, Morelli JN, Henzler T, Buchheidt D, Fink C, Schoenberg SO, et al. 3 Tesla proton MRI for the diagnosis of pneumonia/lung infiltrates in neutropenic patients with acute myeloid leukemia: initial results in comparison to HRCT. Eur J Radiol. 2014;83(1):e61-6.
Figures