0304
LI-RADS category 5 hepatocellular carcinoma: preoperative gadoxetic acid–enhanced MRI to predict early recurrence after curative resection1Department of Radiology, Sichuan University West China Hospital, Chengdu, China
Synopsis
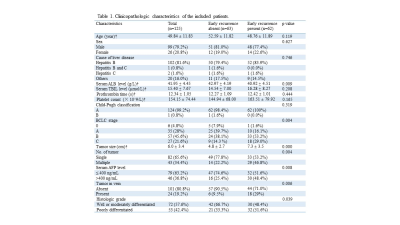
This study aimed to investigate whether LI-RADS v2018 could indicate some prognostic information for high-risk patients with LR-5 hepatocellular carcinoma (HCC). We retrospectively evaluated 125 patients who underwent gadoxetic acid–enhanced MR examination within 1 month before surgical resection for HCC. The Cox proportional hazards model revealed that corona enhancement, peritumoral hypointensity on hepatobiliary phase, multifocality and serum alpha-fetoprotein were independent risk factors for early recurrence. The combined model derived from predictive biomarkers showed good performance, which could be used to effectively predict early recurrence after curative hepatectomy for LR-5 HCC.
Introduction
Could LI-RADS v2018 be possibly indicate some prognostic information for HCC? Prior studies reported that LI-RADS category was associated with postsurgical prognosis of primary hepatic malignancies 1,2. In addition, a recent study reported that some imaging features, including those defined by LI-RADS, could predict microvascular invasion (MVI) and recurrence in high-risk patients with LR-5 HCC 3. However, independent validation of these findings has not yet been performed. Besides, imaging features evaluable in the hepatobiliary phase, which may convey essential prognostic information for LR-5 HCC, were not analyzed in the previous study. Therefore, the purpose of our study was to identify predictive imaging features, including LI-RADS imaging features, in preoperative gadoxetic acid enhanced-magnetic resonance (MR) imaging for the prediction of early recurrence (2 years) after curative resection for LR-5 HCC.Materials and methods
Between July 2015 and July 2018, this retrospective study evaluated consecutive treatment-naïve high-risk patients who underwent gadoxetic acid–enhanced MR examination within 1 month before surgical resection for HCC. Tumor recurrence was determined by clinical and imaging follow-up. All MR images were reviewed by three independent radiologists with respect to the LI-RADS v2018 imaging features, LI-RADS categories and several non-LI-RADS imaging features of all high-risk lesions. The Cox proportional hazards model was used to analyze the predictors for early recurrence after hepatectomy. The performance of the combined prediction model was evaluated by area under the receiver operating characteristic curve (AUC).Results
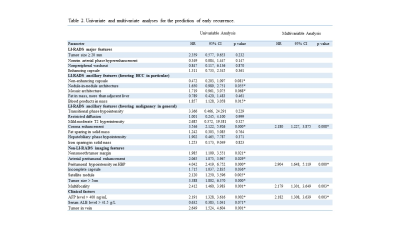
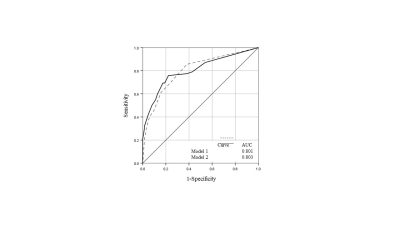
A total of 125 patients (99 men and 26 women, mean age: 49.84 ± 11.83 years) with 164 LR-5 HCCs (mean size: 6.0 ± 3.4 cm) were included; 62 (49.6%) patients experienced tumor early recurrence. The multivariate Cox proportional hazards model revealed that corona enhancement (hazard ratio (HR), 2.180; p = 0.008), peritumoral hypointensity on hepatobiliary phase (HBP) (HR, 2.904; p = 0.000) and multifocality (HR, 2.179; p = 0.003) were independent risk factors for early recurrence. Additional risk factor was serum alpha-fetoprotein (AFP) level > 400 ng/mL (HR, 2.182; p = 0.003). Further, AUC of the obtained Cox regression model was approximately 0.80 for the combination of three predictive imaging biomarkers with or without the integration of AFP.Discussion
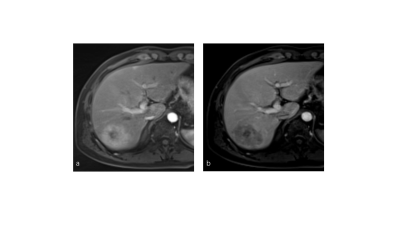
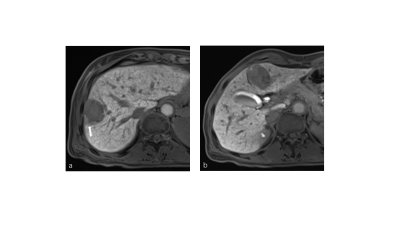
In a single-center retrospective study, we found that one LI-RADS ancillary feature (corona enhancement), one non–LI-RADS feature (peritumoral hypointensity on HBP), multifocality and one clinical factor (serum AFP level > 400 ng/mL) were significant predictors of early recurrence in patients with LR-5 HCC. Hence, none of the LI-RADS major features was found to be independently associated with early recurrence, which is nearly consistent with the previous study 3.Corona enhancement is a radiologic feature of hypervascular, progressed HCC 4. It refers to enhancement of peritumoral parenchyma in the late arterial phase or early portal venous phase; this is attributed to passage of contrast medium from the tumor via the draining sinusoids and portal venules into the surrounding parenchymal hepatic sinusoids 4. Progressed HCCs are apt to invade drainage vessels 4, resulting in intrahepatic metastases or recurrence.
Peritumoral hypointensity on HBP has been reported to be a significant predictor of MVI--a major risk factor for HCC early recurrence after curative therapy 5,6. This corresponds well with our findings. The possible mechanism underlying the appearance of HBP peritumoral hypointensity is the alteration of liver function and diminished uptake of gadoxetic acid in peritumoral hepatocytes, attributing to the disfunction of organic anion-transporting polypeptide transporters on hepatocytes around the tumor due to changes of peritumoral perfusion resulting from MVI 5.
Tumor number and serum AFP level are common, assessable, prognostic factors for HCC postsurgical survival. Studies have shown that patients with multiple tumors are at higher and earlier risk of tumor recurrence compared with those who have single tumor 3,7, which was correspondent with our study. Nevertheless, the data regarding AFP level as a predictor for tumor reccurence varied due to the variance of defined cutoffs in published studies 3,8,9. In our study population, AFP level > 400 ng/mL can be served as a predictive biomarker for early recurrence. However, this finding remains to be validated further in prospective multicenter setting.
Intriguingly, the combined model derived from predictive MR imaging features and MR imaging features along with serum AFP showed comparable performance.
Conclusion
In high-risk patients with LR-5 HCC, preoperative corona enhancement, HBP peritumoral hypointensity, multifocality and serum AFP can be used to effectively predict early recurrence after curative hepatectomy.Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 81771797) and the 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYJC18008).References
1 Choi SH, Lee SS, Park SH, et al. LI-RADS Classification and prognosis of primary liver cancers at Gadoxetic acid-enhanced MRI. Radiology. 2019;290(2):388-397.
2 An C, Park S, Chung YE, et al. Curative resection of single primary hepatic malignancy: Liver Imaging Reporting and Data System Category LR-M portends a worse prognosis. AJR Am J Roentgenol. 2017;209(3):576-583.
3 Chen J, Zhou J, Kuang S, et al. Liver Imaging Reporting and Data System category 5: MRI predictors of microvascular invasion and recurrence after hepatectomy for hepatocellular carcinoma. AJR Am J Roentgenol. 2019;213(4):821-830.
4 Choi JY, Lee JM, Sirlin CB. CT and MR imaging diagnosis and staging of hepatocellular carcinoma: part I. Development, growth, and spread: key pathologic and imaging aspects. Radiology. 2014;272(3):635-654.
5 Lee S, Kim SH, Lee JE, et al. Preoperative gadoxetic acid-enhanced MRI for predicting microvascular invasion in patients with single hepatocellular carcinoma. J Hepatol. 2017;67(3):526-534.
6 Kim KA, Kim MJ, Jeon HM, et al. Prediction of microvascular invasion of hepatocellular carcinoma: usefulness of peritumoral hypointensity seen on gadoxetate disodium-enhanced hepatobiliary phase images. J Magn Reson Imaging. 2012;35(3):629–634.
7 Lee EC, Kim SH, Park H, et al. Survival analysis after liver resection for hepatocellular carcinoma: a consecutive cohort of 1002 patients. J Gastroenterol Hepatol 2017;32(5):1055–1063.
8 An C, Kim DW, Park YN, et al. Single hepatocellular carcinoma: preoperative MR Imaging to predict early recurrence after curative resection. Radiology. 2015;276(2):433-443.
9 Zhang Z, Jiang H, Chen J, et al. Hepatocellular carcinoma: radiomics nomogram on gadoxetic acid-enhanced MR imaging for early postoperative recurrence prediction. Cancer Imaging. 2019 May 14;19(1):22.
Figures