0302
Determining the Value of Fit-for-Purpose MRI Exams of Multiple Sclerosis1Radiology, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States
Synopsis
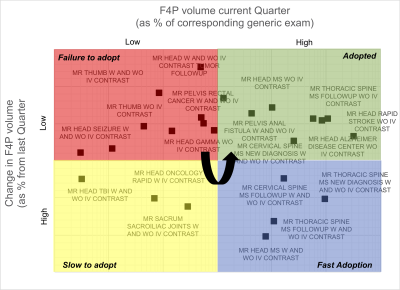
We compare the time savings and reduction in radiologists’ workload after implementing ten new fit-for-purpose MRI protocols for imaging of multiple sclerosis patients at our academic medical center. A 2x2 framework was created to provide a method to monitor implementation of new imaging protocols in order to gauge success of adoption as well as determine areas for operational improvement.
Objective
To determine the value of fit-for-purpose MRI protocols by evaluating their efficiency gains in terms of time savings and reduction of number of images compared to their corresponding generic protocols.Background
Healthcare costs grew unsustainably 3.9% to $3.5 trillion in 2017, accounting for 18% of Gross Domestic Product of the US 1. The traditional fee-for-service model is unable to control costs forcing payors to increasingly adopt value-based healthcare, a care delivery model in which providers, including hospitals and physicians, are paid based on patient health outcomes 2 with the goal to reduce waste and cost 3. Most efforts to reduce costs in radiology have focused on reducing inappropriate utilization 4. Inappropriate examinations also delay timely diagnoses due to the increased workload and potential for burnout among radiologists 5. The department of radiology at our academic medical institute performs 1.2 million procedures annually, offering an unique opportunity to leverage data and technology to prescribe the most appropriate use of imaging tests for given medical condition 6. A total of 38 tailored “fit-for-purpose” (F4P) MRI protocols were created since October of 2017 by select committees of radiologists and technicians. MRI is the targeted modality for efficiency gains due to long exam durations and large variety of protocols. Long scan times are not only costly but are a detriment to patients’ overall satisfaction and reduces their likelihood of undergoing an exam and may even pose harm from unnecessary use of contrast media 7. In this abstract we determine the value of ten Multiple Sclerosis (MS) F4P MRI protocols by evaluating their efficiency gains in terms of time savings and reduction of number of images compared to their corresponding generic protocols previously in use. We also describe a framework for evaluating the adoption of F4P exams that can help guide operational decision-making and strategic interventions.Methods
This project was undertaken as a Quality Improvement Initiative and received exemption by our Institutional Review Board. Exam accession numbers of F4P and corresponding generic exams performed at our institute in the last year were obtained by searching the radiology database using mPower (Nuance Inc., Los Angeles, CA). These were used to retrieve DICOM timestamps and number of files in each exam from the PACS radiology database (Sectra AB, Linköping, Sweden). DICOM scan times were calculated for each exam by calculating the difference of the DICOM timestamps and #DICOM images were calculated and recorded in a CSV file for analyses. Statistical analyses (ANOVA, etc.) were performed in JMP Pro 13 (SAS, Cary, NC). Average and standard errors were calculated and compared to their corresponding generic exams’ values by setting 95% confidence level for significance. A 2x2 matrix plotted the change in F4P volume from last quarter vs. F4P volume from current quarter for a subset of all F4P exam in order to visualize the success of adoption of these F4P exams and to guide actionable decision-making.Results
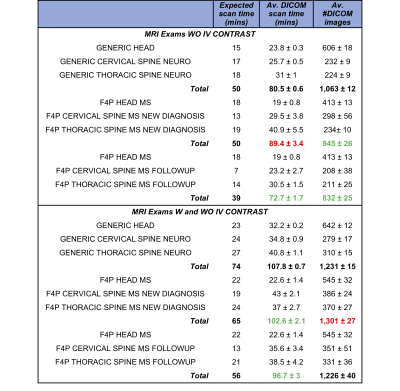
F4P exams without IV contrast for follow up scans were tailored to save 11 minutes from their generic counterpart (Table 1, expected scan time column, 39 min vs. 50 mins) by removing high-resolution scans used to detect infections. Consequently, the F4P new diagnosis remained a 50-min protocol. In practice, this saved on average 8 mins (Table 1, Av. DICOM scan time column, 72.7 vs. 80.5 mins) while the new diagnosis F4P scans added 9 mins. Overall this strategy saved time since follow up exams were performed more often than new diagnosis exams (51 vs. 33 in the last year). Both F4P protocols produced significantly less images to analyze compared to the generic protocol indicating a reduction in radiologists' workload.F4P exams with and without IV contrast for follow up scans were tailored to save 18 minutes from their generic counterpart and the F4P new diagnosis was also reduced by 9 mins by saving time on the cervical spine scans. Although no gains were observed in # files generated, between 5-10% reduction in scan times were achieved in the new diagnosis and follow up F4P scans compared to the original generic protocol.
Figure 1 shows the process by which the F4P adoption diffuses over time (indicated by the curved arrow) among the MRI technicians. Protocols that did not gain traction tend to co-locate in the top left quadrant (red). As these protocols become more utilized, there is an increased change from previous quarter slowly (yellow) then rapidly (blue), finally settling on complete adoption (green quadrant, top right). Location in the blue and green quadrants demonstrates that the MS F4P protocols were rapidly adopted during the last quarter compared to other F4P protocols.
Conclusions
MRI protocols for follow up imaging of MS patients could be tailored to significantly reduce scan time and number of image files, potentially improving patient satisfaction and reducing radiologist workload. A new 2x2 framework provided a method to monitor implementation of new imaging protocols in order to gauge success of adoption as well as determine areas for operational improvement. While methods to improve adoption are being investigated, we expect that identifying early adopters, preferred communication channels, training approaches, and adoption time will be key performance indicators for the successful implementation of F4P protocols.Acknowledgements
No acknowledgement found.References
1. US Center for Medicare and Medicaid Services. NHE Fact Sheet. Updated April 26, 2019. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nhe-fact-sheet.html. Accessed September 16, 2019.
2. NEJM Catalyst. What is the Value-Based Healthcare? Updated January 1, 2017. https://catalyst.nejm.org/what-is-value-based-healthcare/. Accessed September 16, 2019.
3. Boland GW, Glenn L, Goldberg-Stein S, et al. Report of the ACR's Economics Committee on Value-Based Payment Models. J Am Coll Radiol 2017;14:6-14.
4. Duszak R, Berlin JW. Utilization management in radiology, part 1: rationale, history, and current status. J Am Coll Radiol 2012;9:694-9.
5. Chetlen AL, Chan TL, Ballard DH, et al. Addressing Burnout in Radiologists. Acad Radiol 2019;26:526-33.
6. Kuhl CK, Bruhn R, Krämer N, Nebelung S, Heidenreich A, Schrading S. Abbreviated Biparametric Prostate MR Imaging in Men with Elevated Prostate-specific Antigen. Radiology 2017;285(2):493-505.
7. Stratta P, Canavese C, Aime S. Gadolinium-enhanced magnetic resonance imaging, renal failure and nephrogenic systemic fibrosis/nephrogenic fibrosing dermopathy. Curr Med Chem 2008;15:1229-35.
Figures