0299
Rapid High-Value Diagnostic and Quantitative Knee MRI: A Prospective Artificial Intelligence Study1Stanford University, Stanford, CA, United States, 2Santa Clara Valley Medical Center, San Jose, CA, United States, 3LVIS Corporation, Palo Alto, CA, United States, 4Harvard Medical School, Boston, MA, United States
Synopsis
Knee MRI protocols usually require 20+ minutes of scan time, leading to great interest in expedited and high-value imaging examinations. Moreover, despite the popularity of quantitative imaging for osteoarthritis, it is not routinely implemented clinically. In this study, we use a 5-minute quantitative double-echo steady-state (qDESS) sequence that produces simultaneous morphological images and T2 relaxation time measurements. We prospectively enhance the slice-resolution of qDESS using deep learning. We show that qDESS provided high diagnostic accuracy compared to both diagnostic knee MRI and surgical findings. Additionally, automatic T2 maps increased reader diagnostic confidence and sensitivity to cartilage lesions.
Introduction
Knee MRI protocols usually require 20+ minutes of scan time, leading to interest in high-value expedited protocols1. Moreover, despite the popularity of quantitative imaging for osteoarthritis, common quantitative measures such as the T2 relaxation time are not routinely implemented clinically2,3. The quantitative double-echo in steady-state (qDESS) pulse sequence may expedite knee MRI while simultaneously providing T2 relaxation times4,5. qDESS generates a T2/T1-weighted (S+) echo and more highly T2-weighted (S-) echo6–8. The two echoes can be used for accurate T2 mapping9,10. In this study, we evaluate the clinical utility of the multi-contrast and quantitative 5-minute qDESS sequence, compared to conventional imaging and arthroscopy. We additionally implemented deep-learning-based super-resolution (DLSR) to enhance the slice resolution of prospectively-sampled qDESS11.Methods
100 consecutive patients referred for routine knee MRI examinations by physicians were included in this study. A 5-minute sagittal water-excitation 3D-qDESS sequence was added to the diagnostic knee MRI protocol consisting of five 2D FSE sequences. MRI scanning was performed on Discovery MR750 3.0T MRI scanners (GE Healthcare, Waukesha, Wisconsin) using an 8-channel transmit-receive knee coil (InVivo, Gainesville, Florida). qDESS was acquired with 1.6mm slice-resolution and Fourier interpolated to 0.8mm thickness using the “ZIP2” option in 51 patients, and acquired with 0.8mm slice-resolution in the remaining 49 patients (additional parameters: matrix=416x512, field-of-view=160mm, TE/TR= 6/18ms, flip-angle=20°, parallel imaging=2x1). qDESS image reconstruction and T2 relaxation map creation were performed immediately on the scanner computer.DLSR was used to improve the ZIP2 Fourier interpolation image quality11. DLSR was trained to provide twofold enhancement in slice resolution from 1.6mm to 0.8mm using 49 of the 100 qDESS patient scans that were acquired with 0.8mm slice-resolution (34/10/5 scans for training/validation/testing). This network was pre-trained using DESS scans from the Osteoarthritis Initiative (124/35/17 scans for training/validation/testing)11.
DLSR was applied to the remaining 51 of the 100 patients scanned prospectively with 1.6mm qDESS slices. These were independently reviewed by an experienced musculoskeletal radiologist and third-year radiology resident. Both readers first reviewed the conventional imaging protocol and after a two-month washout period, reviewed qDESS images. During the qDESS review, the readers first reviewed the two morphological images, then qDESS with the T2 maps. Following the qDESS+T2 readings, the readers assessed the added diagnostic utility of including a coronal proton-density-weighted fat-saturated (PD-FS) sequence. The readers also scored the diagnostic quality of the protocols (1=none, 2=poor, 3=acceptable, 4=good, 5=very good).
The following abnormalities were evaluated: Ligaments (cruciate and collateral): low/moderate sprain, or complete tear; Menisci: myxoid degeneration or horizontal/radial/vertical/longitudinal/complex/complex-flap tears; Cartilage: grade 1/2A/2B/3 lesions (modified Noyes criteria)12,13; Bone: bone marrow edema (BME), subchondral cyst, or fracture; Extensor Mechanism: partial/complete tear; Synovium: effusion or synovitis. Cartilage and osseous abnormalities were evaluated in the medial and lateral femoral condyles and tibial plateaus, femoral trochlea, and patella.
Surgery was performed on 43 of 51 patients by orthopedic surgeons, who documented cartilage lesions according to the Noyes criteria, full thickness anterior and posterior cruciate ligament tears, meniscal tears, and synovitis.
The agreement and 95% confidence intervals (CI) between the conventional imaging protocol and qDESS findings, and the area under the receiver operating curve (AUC) were calculated. The added agreement from the inclusion of the T2 maps and the PD-FS sequence was evaluated. The sensitivity, specificity, and AUC of the conventional knee MRI sequences and the qDESS scans (with/without T2 maps) were computed with respect to surgical findings. Differences in these metrics for qDESS and conventional imaging were tested using exact McNemar tests (α=0.05). Cohen’s Kappa was used to evaluate inter-observer agreement.
Results
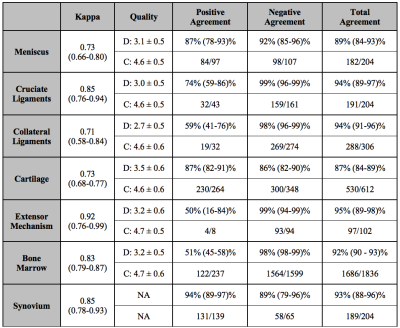
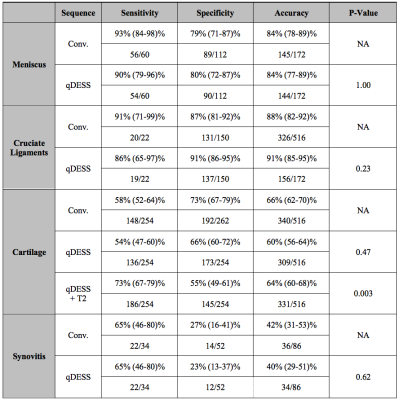
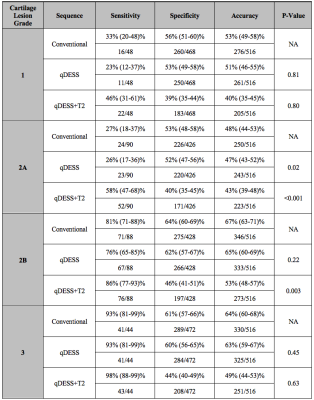
51 patients (34/17 male/female, mean age:44±18 years, range:18-98 years) were evaluated by the readers. Agreement and AUC (0.91) between findings from the conventional imaging protocol and the qDESS sequence was high, along with inter-reader agreement (Fig.1).qDESS had comparable sensitivity and specificity (AUC = 0.60) to conventional imaging (AUC = 0.65) for meniscal and cruciate ligaments injuries (Fig.2), but higher sensitivity for cartilage lesions. Including a qDESS T2 map (AUC = 0.64) changed the diagnosis or diagnostic confidence in 41/51 patients and in 38% of all cartilage surfaces evaluated. qDESS+T2 mapping had higher sensitivity for grade 1 and 2A lesions compared to the conventional imaging, (Fig.3). Including a coronal PD-FS sequence increased sensitivity to osseous abnormalities from 45% (37-54%) to 68% (59-75%).
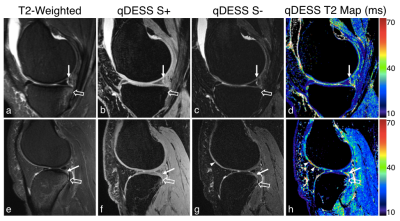
Example qDESS and routine MR images showed high conspicuity for arthroscopically-confirmed peripheral and oblique meniscal tears (Fig.4-5, respectively). Both patients examples depicted normal-appearing cartilage on morphologic images but focal changes on qDESS T2 maps.
Discussion
qDESS demonstrated high concordance with findings from a conventional diagnostic knee MRI protocol and demonstrated comparable accuracy to the conventional protocol compared with arthroscopy. The automatic T2 maps improved reader diagnostic confidence and enhanced the detection of subtle cartilage lesions, even in otherwise morphologically normal-appearing cartilage. While T2 maps decreased cartilage lesion specificity, this may occur because even arthroscopy may not depict the earliest signs of cartilage degeneration14. 94% of incorrect qDESS ligament findings were sprains and 50% were myxoid degeneration, which would not affect the standard of care for patients.Conclusion
A rapid, high-resolution, and multi-contrast qDESS sequence with automatic T2 mapping and a prospective deep-learning-based super-resolution enhancement provided high diagnostic accuracy compared to the diagnostic knee MRI protocol and arthroscopy.Acknowledgements
We would like to acknowledge our funding sources: National Institutes of Health (NIH) grant numbers NIH R01 AR063643, R01 EB002524, K24 AR062068, and P41 EB015891. GE Healthcare, Philips, and Stanford Medicine Precision Health and Integrated Diagnostics.References
1. van Beek, E. J. R. et al. Value of MRI in medicine: More than just another test? J. Magn. Reson. Imaging 49, e14–e25 (2019).
2. Baum, T. et al. Cartilage and meniscal T2 relaxation time as non-invasive biomarker for knee osteoarthritis and cartilage repair procedures. Osteoarthritis Cartilage 21, 1474–84 (2013).
3. Kijowski, R., Blankenbaker, D. G., Munoz Del Rio, A., Baer, G. S. & Graf, B. K. Evaluation of the articular cartilage of the knee joint: value of adding a T2 mapping sequence to a routine MR imaging protocol. Radiology 267, 503–13 (2013).
4. Chaudhari, A. S. et al. Five-minute knee MRI for simultaneous morphometry and T 2 relaxometry of cartilage and meniscus and for semiquantitative radiological assessment using double-echo in steady-state at 3T. J. Magn. Reson. Imaging 47, 1328–1341 (2018).
5. Chaudhari, A. S. et al. Combined 5-minute double-echo in steady-state with separated echoes and 2-minute proton-density-weighted 2D FSE sequence for comprehensive whole-joint knee MRI assessment. J. Magn. Reson. Imaging 1–12 (2018). doi:10.1002/jmri.26582
6. Bruder, H., Fischer, H., Graumann, R. & Deimling, M. A new steady-state imaging sequence for simultaneous acquisition of two MR images with clearly different contrasts. Magn. Reson. Med. 7, 35–42 (1988).
7. Redpath, T. W. & Jones, R. A. FADE--a new fast imaging sequence. Magn Reson Med 6, 224–234 (1988).
8. Lee, S. Y. & Cho, Z. H. Fast SSFP gradient echo sequence for simultaneous acquisitions of FID and echo signals. Magn Reson Med 8, 142–150 (1988).
9. Welsch, G. H. et al. Rapid estimation of cartilage T2 based on double echo at steady state (DESS) with 3 Tesla. Magn. Reson. Med. 62, 544–9 (2009).
10. Sveinsson, B., Chaudhari, A., Gold, G. & Hargreaves, B. A simple analytic method for estimating T2 in the knee from DESS. Magn. Reson. Imaging 38, 63–70 (2017).
11. Chaudhari, A. S. et al. Super-resolution musculoskeletal MRI using deep learning. Magn. Reson. Med. 80, 2139–2154 (2018).
12. Noyes, F. R. & Stabler, C. L. A system for grading articular cartilage lesions at arthroscopy. Am. J. Sports Med. 17, 505–513 (1989).
13. Kijowski, R. et al. Knee joint: comprehensive assessment with 3D isotropic resolution fast spin-echo MR imaging--diagnostic performance compared with that of conventional MR imaging at 3.0 T. Radiology 252, 486–495 (2009).
14. Kretzschmar, M. et al. Spatial distribution and temporal progression of T2 relaxation time values in knee cartilage prior to the onset of cartilage lesions – data from the Osteoarthritis Initiative (OAI). Osteoarthr. Cartil. 27, 737–745 (2019).
Figures