0277
USPIO-enhanced MRI for pre-operative lymph node staging after neoadjuvant chemoradiotherapy in esophageal cancer1surgery, Radboudumc, Nijmegen, Netherlands, 2radiology and nuclear medicine, Radboudumc, Nijmegen, Netherlands, 3radiology, Osaka University Graduate School of Medicine, Osaka, Japan
Synopsis
Lymph node dissections during esophagectomy may be omitted or minimized in patients with esophageal cancer without or with limited lymph node metastases, thereby reducing associated morbidity. A promising technique to detect lymph node metastases is T2*-weighted MRI after the injection of ultrasmall superparamagnetic iron oxide nanoparticles (USPIO, ferumoxtran-10). The aim of this study is to evaluate the feasibility of USPIO-enhanced MRI in the detection of locoregional lymph node metastases in patients with esophageal cancer whom underwent nCRT, and to study the effect of nCRT on the evaluation of USPIO-enhanced MRI.
Background
In 69% of patients suffering from operable esophageal cancer, no metastatic lymph nodes are found after neoadjuvant chemoradiotherapy (nCRT)1. Ideally, extensive lymph node dissections during esophagectomy should be omitted or minimized in these patients to reduce associated morbidity. T2*-weighted MRI with ultrasmall superparamagnetic iron oxide nanoparticles (USPIO, ferumoxtran-10) has been proven to be a valuable imaging technique to detect lymph node metastases2. Lymph nodes without nanoparticles retain MR signal intensity, an indication for abnormal nodal status and thus suspicion for malignancy. Normal lymph nodes accumulate nanoparticles, causing strong MR signal attenuation. Contrary to other diagnostic modalities, USPIO-enhanced MRI has an excellent spatial resolution to detect small lymph nodes, e.g. reaching short axis diameters <3 mm in prostate cancer3. For esophageal cancer, USPIO-enhanced MRI is more challenging due to the location of the lymph nodes close to the heart and lungs. The aim of this study is to assess the feasibility of USPIO-enhanced MRI in the detection of locoregional lymph node metastases in patients with esophageal cancer before, as well as after nCRT.Method
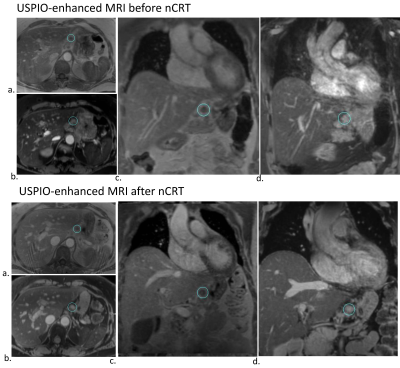
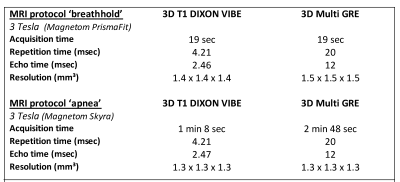
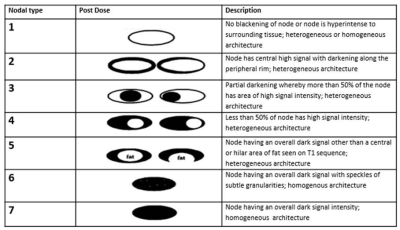
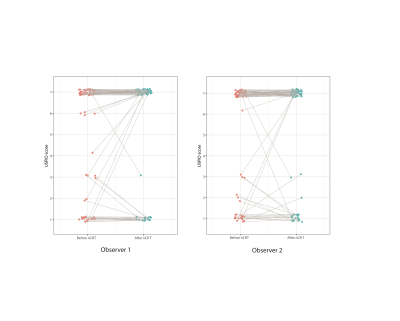
The study is a prospective, single centre, feasibility study in patients undergoing minimally invasive esophagectomy with suspected lymph node metastases. USPIO-nanoparticles (Ferumoxtran-10, 2.6 mg Fe/kg body weight) were intravenously infused 24 to 36 hours before MRI. All patients underwent a USPIO-enhanced MRI examination with multiple breathholds before nCRT (3T Magnetom PrismaFit, Siemens Healthcare, Erlangen, Germany). The MR sequences are described in figure 1. After nCRT (~3 months), USPIO-enhanced MRI was repeated on the day of surgery with the patient under controlled prolonged apnea of four minutes in a 3T MR system (Magnetom Skyra, Siemens Healthcare) in a hybrid operation room. 3D T1-weighted Dixon and water-selective iron-sensitive multi gradient echo sequences were used to visualize suspicious esophageal lymph nodes. T2*-weighted iron-sensitive scans enabled the visualization of the presence or absence of nanoparticles in the lymph nodes (figure 1). The MRI images from both pre-nCRT and post-nCRT examinations were analyzed independently by two experienced radiologists using adapted diagnostic guidelines proposed by Anzai et al4 (figure 2). Lymph nodes with a full or partial high signal intensity were considered suspicious (score 1-4) and lymph nodes with overall dark intensity or lymph nodes with fatty hilum were considered not suspicious for metastases (score 5-7). The inter-observer variation between radiologists was calculated with kappa statistics and was performed using R (version 3.2.1).Results
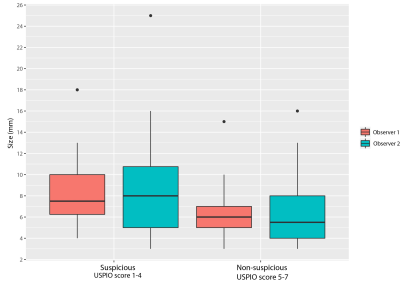
15 patients were enrolled in the study and underwent a pre-nCRT USPIO-enhanced MRI examination. Five patients developed distant metastases after nCRT, and did not undergo surgery and a second USPIO-enhanced MRI scan. From 15 patients, a total of 435 lymph nodes were evaluated by the first radiologist with a mean short axis length of 5 mm (range 2-18) and 233 lymph nodes by the second radiologist with a mean short axis length of 6 mm (range 2-25). 193 lymph nodes could be matched and were evaluated by both radiologists. The size of the lymph nodes compared to the USPIO scores is visualized in figure 3. 75% of the matched nodes received the same score by both radiologists, with corresponding kappa value for inter-observer agreement of 0.57 (P = 0.044). In 10 patients USPIO-enhanced MRI was made before and after nCRT. In these patients, 72 nodes were analyzed by both radiologists before and after nCRT. From these matched nodes, 5 (observer 1) and 3 (observer 2) out of 22 suspicious nodes before nCRT received a non-suspicious score after nCRT (figure. 4). 66 (observer 1) and 67 (observer 2) out of the 72 matched lymph nodes had the same USPIO score before and after nCRT.Discussion
In this feasibility study, we showed that USPIO nanoparticles accumulate in regional lymph nodes of esophageal cancer before and after nCRT. In absence of previous experience of scoring USPIO-enhanced MRI in esophageal cancer, the high agreement between two independent radiologists is remarkable. Generally, lymph nodes shrink as a result of nCRT, but their appearance on USPIO-enhanced MRI remains the same in the majority of the lymph nodes. Suspicious nodes remain suspicious, which could either represent residual metastases in nodes after nCRT, or fibrotic tissue obstructing the accumulation of (macrophages loaded with) nanoparticles. Future correlation to pathology on a node-to-node level could resolve this and will be used to validate the nodal characterization of USPIO-enhanced MRI in esophageal cancer.Conclusion
We performed USPIO-enhanced MRI before and after nCRT in patients with esophageal cancer. After nCRT, MRI with controlled mechanical ventilation was safe and feasible and USPIO uptake in regional lymph nodes was seen on T2*-weighted sequences in all patients. Radiological evaluation of lymph nodes on T2*-weighted MRI was done with high interobserver agreement. The technique might be of added value in the decision to start nCRT, in monitoring the response of nCRT, and in the surgical treatment plan. Correlation to pathology is needed to make a definitive assessment on the performance of USPIO-enhanced MRI for esophageal cancer.Acknowledgements
No acknowledgement found.References
1. van Hagen P, Hulshof MC, van Lanschot JJ, et al: Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 366:2074-84, 2012
2. Fortuin AS, Bruggemann R, van der Linden J, et al: Ultra-small superparamagnetic iron oxides for metastatic lymph node detection: back on the block. Wiley Interdiscip Rev Nanomed Nanobiotechnol 10, 2018
3. Birkhauser FD, Studer UE, Froehlich JM, et al: Combined ultrasmall superparamagnetic particles of iron oxide-enhanced and diffusion-weighted magnetic resonance imaging facilitates detection of metastases in normal-sized pelvic lymph nodes of patients with bladder and prostate cancer. Eur Urol 64:953-60, 2013
4. Anzai Y, Piccoli CW, Outwater EK, et al: Evaluation of neck and body metastases to nodes with ferumoxtran 10-enhanced MR imaging: phase III safety and efficacy study. Radiology 228:777-88, 2003
Figures