0246
Compressed Sensing with and without Deep Learning Reconstruction: Comparison of Capability for Improving Lumber Spine MRI with Parallel Imaging1Radiology, Fujita Health University School of Medicine, Toyoake, Japan, 2Canon Medical Systems Corporation, Otawara, Japan, 3Radiology, Department of Radiology, Fujita Health University Hospital, Toyoake, Japan, 4Radiology, Joint Research Laboratory of Advanced Medical Imaging, Fujita Health University School of Medicine, Toyoake, Japan
Synopsis
There have been no major reports for assessing the utility of compressed sensing (CS) and deep learning reconstruction (DLR) as compared with routinely applied parallel imaging (PI) on lumber spine MRI. We hypothesized that CS with DLR was able to improve image quality and shorten examination time on lumber spine MRI, when compared with PI. The purpose of this study was to directly compare the capability for improving lumber spine MRI among CS with and without DLR and PI in patients with different lumber spinal diseases.
Introduction
As further examination, lumber spine MR imaging (MRI) is widely applied in routine clinical practice, and increased number of lumber spin MR examination requires decreasing examination time without reducing image quality. Improving the temporal and spatial resolution on lumber spine MRI have been tried to using not only image domain based parallel imaging (PI) techniques, but also k-space domain based parallel imaging technique at 1.5 and 3 Tesla (T) MR systems (1), although PI is currently suggested as having the limited capability for these clinical purposes. In this situation, compressed sensing (CS) is one of the newly proposed methods for aiming to reduce the number of k-space samples by exploiting compressibility or sparsity in an appropriate transform domain (2). However, one of the drawbacks of CS is suggested as relatively lower SNR than PI. Therefore, deep learning reconstruction (DLR) is also proposed for improving imaging quality of MRI in different regions (3). However, there have been no major reports for assessing the utility of CS and DLR as compared with routinely applied PI on lumber spine MRI. We hypothesized that CS with DLR was able to improve image quality and shorten examination time on lumber spine MRI, when compared with PI. The purpose of this study was to directly compare the capability for improving lumber spine MRI among CS with and without DLR and PI in patients with different lumber spinal diseases.Materials and Methods
Thirty consecutive lumber spinal disease patients (mean age 68.6 years, range 34–86 years) with various lumber spinal diseases underwent T2-weighted imaging at 3T MR system (Vantage Galan 3T, Canon Medical Systems, Otawara, Japan) by image domain based PI (SPEEDER, Canon Medical) and CS (Compressed SPEEDER, Canon Medical). Acceleration factors of PI and CS were 1.5 and 3 in this study. Then, all CS images were reconstructed with and without DLR. As quantitative image quality indexes in each patient, SNR of vertebra, percentage of coefficient of variation (%CV) of vertebra and contrast–to–noise ratio (CNR) between vertebra and spinal cord were determined by ROI measurement. For qualitative image quality assessment in each patient, two radiologists evaluated overall image quality, artifacts and diagnostic confidence by 5–point visual scoring system, and final value of each qualitative index was made by consensus of two readers. To compare quantitative image quality indexes among three methods, SNR, %CV and CNR were compared among CS with and without DLR and PI by Wilcoxon signed-rank test. For evaluating inter-observer agreement of each qualitative index, weighted-kappa statistics and c2test was performed. To compare each qualitative index among three methods, each index was also compared among CS with and without DLR and PI by Wilcoxon signed-rank test. Finally, mean examination time was also compared among CS with and without DLR and PI by Tukey’s HSD test .Results
Representative case is shown in Figure1. When compared each quantitative image quality index among three methods, there were no significant differences of SNR, %CV and CNR among CS with and without DLR and PI (p>0.05). The result of inter-observer agreement for each qualitative image quality index between two readers is shown in Figure 2. Inter-observer agreements for overall image quality and artifact of CS with and without DLR (0.74≤κ≤0.79, p<0.0001) were substantial, although those of PI were almost perfect (κ=0.90, p<0.0001). Figure 3 shows the results of compared each qualitative image quality index among three methods. Overall image quality and artifact scores of CS with DLR (overall image quality: 4.7±0.1, p=0.02; artifact: 1.4±1.1, p=0.03) and PI (overall image quality: 4.8±0.1, p=0.01; artifact: 1.2±1.1, p=0.002) were significantly higher than that of CS without DLR (overall image quality: 4.4±0.1, artifact: 1.8±1.1). On the other hand, there were no significant differences of diagnostic confidence among CS with and without DLR and PI (p>0.05). Figure 4 shows the results of compared examination time among three methods. Mean examination time had significant difference among three methods (p<0.0001). In addition, all mean examination times were as follows: CS with DLR, 114.8±3.4s; CS without DLR, 107.3±3.4s; PI, 207.6±3.4s.Conclusion
CS is able to significantly reduce examination time than PI, and DLR has a potential to improve image qualities of MR imaging obtained with CS. When compared with PI, combination of CS and DLR makes it possible to improve lumber spine MR examination in routine clinical practice.Acknowledgements
No acknowledgement found.References
- Deshmane A, Gulani V, Griswold MA, Seiberlich N. J Magn Reson Imaging. 2012 Jul;36(1):55-72.
- Feng L, Benkert T, Block KT, Sodickson DK, Otazo R, Chandarana H. J Magn Reson Imaging. 2017 Apr;45(4):966-987.
- Kidoh M, Shinoda K, Kitajima M, et al. Magn Reson Med Sci. 2019 Sep 4. doi: 10.2463/mrms.mp.2019-0018. [Epub ahead of print]
Figures

Figure 1. 58-year-old male patient with lumber disk herniation (L to R: CS with DLR and CS without DLR and PI).
Image quality on CS without DLR are slightly lower than those of others, especially visualizations of Th12, L4 and L5 vertebra bodies (arrows). Mean SNRs of CS with and without DLR and PI were as follows: 11.9, 10.9 and 15.5. Overall image qualities in this case were as follows: CS with DLR. 5; CS without DLR, 4; PI, 5.
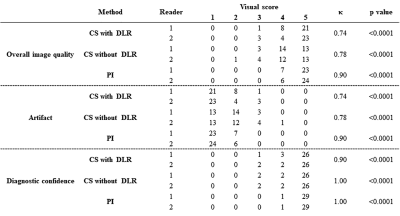
Figure 2. Results of inter-observer agreement for each qualitative image quality index between two readers on three methods.
On each qualitative image quality, inter-observer agreements for overall image quality and artifact of PI and CS without DLR on three methods were assessed as follows: CS with DLR, 0.74≤κ≤0.90; CS without DLR, 0.78≤κ≤1.00; PI: 0.90≤κ≤1.00.
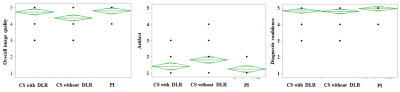
Figure 3. Results of comparison for all qualitative image quality indexes among three methods.
Overall image quality and artifact scores of PI and CS with DLR were significantly better than those of CS without DLR (p<0.0001), although there was no significant difference among PI and CS with and without DLR.
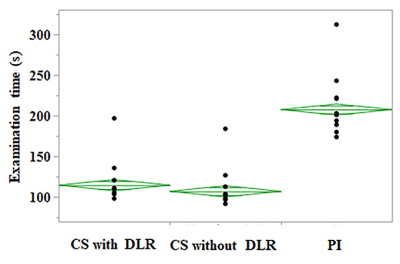
Figure 4. Results of compared mean examination time among three methods.
Mean examination times of CS with DLR (114.8±3.4s), CS without DLR (107.3±3.4s) and PI (207.6±3.4s) had significant differences (p<0.0001).