0239
Disconnectome-Symptom Mapping in Traumatic Brain Injury: Application to Paediatric Populations1School of Life & Health Sciences & Aston Neuroscience Institute, Aston University, Birmingham, United Kingdom, 2Clinical Sciences, Murdoch Children’s Research Institute, Melbourne, Australia, 3School of Psychology, Deakin University, Geelong, Australia
Synopsis
Disconnectome-symptom mapping (DSM) was used to identify relationships between brain and behaviour, by assessing the effect of pathology-intersected white matter tracts on neuropsychological outcomes. This study used DSM to see how IQ, two years post-injury, related to disconnections in the brain, following paediatric traumatic brain injury. For this, two approaches were employed: the BCBtoolkit, designed for use in adults, and a child-analogue. This study found the BCBtoolkit to be less sensitive than the child-analogue, however, in both methods, disconnections in the superior longitudinal fasciculus and external capsule correlated with a reduced IQ when comparing disconnected patients to controls.
Introduction
Lesion-symptom mapping (LSM) is a valuable approach used to identify brain-behaviour relationships, by localising areas of pathology directly related to deficits in cognitive function1. However, these approaches fail to consider the white matter tracts damaged/disconnected as a result of pathology, that may have implications on cognition/behaviour2. This study therefore incorporated disconnected tracts into LSM approaches (Disconnectome-Symptom Mapping, DSM) to explore how a deficit in IQ, two years post-injury, related to disconnections in the brain following paediatric traumatic brain injury (pTBI). Two approaches were compared: the BCBtoolkit3, software allowing DSM through the use of an adult template/tractograms, and a child-analogous method.Methods
This study consisted of 52 children, 17 of whom had TBI lesions (mean age = 9.7 yrs, range = 5.9 – 13.7 yrs), and 35 were typically developing (TD) controls (mean age = 10.6 yrs, range = 6.5 – 15.5 yrs). All participants had scans acquired on a 3T Siemens Trio scanner using a 32-channel head-coil, on average five weeks post-injury. All participants had a sagittal 3D T1-weighted (T1w) scan (MPRAGE, TR = 1900 ms, TE = 2.15 ms, IR prep = 900 ms, parallel imaging factor (GRAPPA) 2, flip angle 9 degrees, BW 200 Hz/px, 176 slices, resolution 1.0 x 0.5 x 0.5 mm). In addition, 19 of the 35 TD controls, had axial 2D single-shot echo-planar images acquired (TR = 9300 ms, TE = 104 ms, flip angle 90 degrees, 64 slices, resolution 2.0 x 2.0 x 2.0 mm, with 60 diffusion-encoding gradient directions (b = 2000 s/mm2) and 10 images acquired with no diffusion weighting (b = 0 s/mm2)). Lesions were manually delineated on patients’ T1w scans.For the BCBtoolkit approach, all TBI patients’ T1w scans and lesion-masks were non-linearly registered to MNI152 space, via enantiomorphic filling3. For each patient, the lesion-intersecting tracts were found from each of ten healthy adult control tractograms (provided by BCBtoolkit), and were further binarised and transformed into percentage overlap (diconnectome) maps.
An age- and sex-matched T1w brain template (1.0 mm3), was generated for the child-analogue approach using Template-O-Matic4 (SPM8, MATLAB R2012a). Anatomically constrained tractography (ACT) was performed using MRtrix3.0 for each of the 19 TD controls. Disconnectome maps were produced by replicating the BCBtoolkit steps using the paediatric template/tractograms.
The AnaCOM2 tool of the BCBtoolkit was used for DSM in both approaches5. This identified clusters of disconnections that were associated with a reduction in IQ, when comparing patients to TD controls. For each cluster, three groups of subjects exist: disconnected patients, spared patients and TD controls. Kruskal-Wallis tests were performed to examine whether patients and controls had the same distribution of IQs. Post-hoc Mann-Whitney comparisons were then made between groups for each cluster. All p-values were Bonferroni-Holm corrected for multiple comparisons.
Results
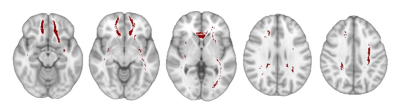
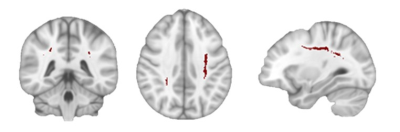
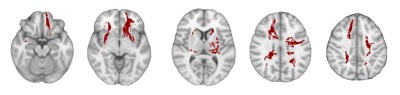
For the BCBtoolkit approach, a comparison of all three groups, at each cluster, found eight clusters with a significant difference between subjects’ IQs (Figure 1). Post-hoc comparisons between disconnected patients and controls, found one cluster, mainly located in the left superior longitudinal fasciculus (SLF), to have significantly different IQs between groups (p = 0.04, r = -0.46) (Figure 2). The estimated effect sizes for this and one other cluster (p = 0.07, r = -0.41) were of a moderate size, and were mainly located in the left SLF, the right external capsule, and the corpus callosum (CC).The child-analogue approach found 24 clusters with a significant difference between subjects’ IQs (Figure 3), however, post-hoc comparisons found no significant differences between the IQs of disconnected patients and TD controls. Five clusters had moderate-to-large effect sizes (r ≥ -0.43), being mainly located in the left/right external capsule and the left/right SLF.
Discussion
This study found moderate-to-large effects in the SLF or external capsule when comparing disconnected patients to TD controls, supporting the idea that DSM is a useful approach for examining the widespread brain changes and functional impairments that may occur in pTBI. The significance of findings were dependent upon the approach. However, the presence of moderate-to-large effect sizes in similar regions using both approaches, suggested that there may be a relationship between disconnections in these areas in pTBI and a reduction in IQ, two years post-injury. Previous research shows a relationships between SLF tract integrity and IQ in children6,7, corroborating the findings reported here. The use of paediatric template/tractograms resulted in disconnectome maps having a larger volume, therefore encapsulating the larger variability in the quantity and direction of tracts observed in children. As a result, more clusters were generated, spanning a larger area when compared to the BCBtoolkit approach. Taken together, these findings suggest that structural MRI scans can be used to assess the relationship between areas of lesion-induced white matter disconnections and IQ in pTBI. This heralds new opportunities to examine brain-behaviour relationships in rare, paediatric clinical samples.Conclusion
This study has two main findings: first, that the method used to assess DSM will affect the results. Secondly, that disconnections in the SLF and external capsule have an effect when comparing the IQs of disconnected patients with controls. Future research should focus on using the child-analogue approach, with larger sample sizes, to further investigate this study’s novel findings.Acknowledgements
The work in this project is supported by a European Consolidator Fellowship to AGW (PROBIT: 682734). AS was supported by a PhD studentship from PROBIt and Aston University’s Prize studentship scheme.References
1. Bates E, Wilson SM, Saygin AP, et al. Voxel-based lesion–symptom mapping. Nat Neurosci [online serial]. Epub 2003.:11–12.
2. Geschwind N. Disconnexion syndromes in animals and man: Part I. Brain [online serial]. 1965;88:237.
3. Foulon C, Cerliani L, Kinkingnéhun S, et al. Advanced lesion symptom mapping analyses and implementation as BCBtoolkit. Gigascience. 2018;7(3):1–17.
4. Wilke M, Holland SK, Altaye M, Gaser C. Template-O-Matic: A toolbox for creating customized pediatric templates. Neuroimage [online serial]. 2008;41:903–913.
5. Kinkingnéhun S, Volle E, Pélégrini-Issac M, et al. A novel approach to clinical-radiological correlations: Anatomo-Clinical Overlapping Maps (AnaCOM): Method and validation. Neuroimage [online serial]. 2007;37:1237–1249.
6. Urger SE, De Bellis MD, Hooper SR, Woolley DP, Chen SD, Provenzale J. The superior longitudinal fasciculus in typically developing children and adolescents: Diffusion tensor imaging and neuropsychological correlates. J Child Neurol [online serial]. 2014;30:9–20.
7. Schmithorst VJ, Wilke M, Dardzinski BJ, Holland SK. Cognitive Functions Correlate With White Matter Architecture In A Normal Pediatric Population: A Diffusion Tensor MR Imaging Study. Hum Brain Mapp [online serial]. 2005;26:139–147.
Figures