0226
Prematurity-related brain injuries disrupt thalamocortical reciprocal growth1USC Stevens Neuroimaging and Informatics Institute, Keck School of Medicine of USC, University of Southern California, Los Angeles, CA, United States, 2Department of Radiology and Biomedical Imaging, UCSF School of Medicine, University of California, San Francisco, San Francisco, CA, United States
Synopsis
Prematurity-related injuries often result in aberrant brain maturation, specifically on peri-thalamic white matter. We investigated the effects of these injuries on the intra-thalamic tissue integrity and on thalamocortical connectivity. We found that injuries did not substantially affect thalamic volume or thalamic DTI parameters, but did have a substantial effect on the correlative growth between the thalamus and cortex. This implies that brain injuries disrupt the reciprocal development of the thalamus and cortex, which may indicate abnormal thalamocortical connectivity.
Introduction
Thalamocortical development is characterized by ascending thalamic axons meeting their descending cortical axons simultaneously, with each guiding the growth of the other.1 However, preterm birth often results in aberrant brain maturation, due to prematurity-related injuries on peri-thalamic areas including the white matter. The overarching goal of our research was to investigate whether peri-thalamic injuries affects thalamic growth and myeloarchitecture in preterm neonates, and to assess whether such injuries affects reciprocal growth between the cortex and thalamus.Methods
SubjectsOur dataset comprises of 127 preterm neonates, admitted to the UCSF Benioff Children’s Hospital of San Francisco between June 2011 and November 2018. The babies were scanned twice: first within 2 weeks after birth, then near their term-equivalent age before discharge from the hospital. Many scans were excluded from the final dataset due to: (i) a large amount of motion artifacts, or (ii) evidence of congenital malformation. Parental consent was obtained for all cases following a protocol approved by the Institutional Committee on Human Research. The final dataset contained 92 preterm neonates and 113 scans (mean gestational age at birth = 27.9 weeks; age at scan: range 28.8-43.2 weeks).
Neuroimaging Data
Acquisition Newborns were scanned on a 3-Tesla General Electric Discovery MR750 system. Customized MRI-compatible incubators with specialized head coils were used to provide a quiet, well-monitored environment for neonates during the MRI scan, minimizing patient movement and improving the signal-to-noise ratio. T1-weighted images were acquired using sagittal 3D IR-SPGR (TR=min; TE=min; inversion time of 450 ms; FOV=180×180 mm2; NEX=1.00; FA=15°), yielding images with 0.7×0.7×1mm3 resolution.
Evaluation of prematurity-related brain injury
Patients were separated into two groups: those with injury and those without. Brain injuries were visually scored by expert radiologist, and all MRI scans were labeled either into no injury group (No) or injury group (Inj) if any type of injury fell within the mild-severe grade range for all types of injuries (intraventricular hemorrhage, and white matter injuries). Within the injury group, patients were further subdivided into those with intraventricular hemorrhaging (IVH) and those with white matter injuries (WMI) (IVH = 14 patients, WMI = 8).
Data Processing and Analysis
The thalamic borders and landmarks are poorly defined on preterm neonatal MRI. Therefore, conventional segmentation protocols and tools, which focus on adult thalamus segmentation, are ineffective in our line of research.2 To overcome this issue, we manually segmented 40 neonatal thalami using the sub-cortical gray matter seen on T2-weighted images and white matter tracts seen on DTI-FA maps. These manual segmentations were used to train an automated segmentation based on a multi-atlas and label fusion technique.3 A rater evaluated all segmentations visually and manually corrected as needed prior to data analyses.
Statistical Analysis
We used general linear models (GLM) to assess changes in relation to a specific clinical variable while considering gestational age (GA) at birth as a covariate. We performed group comparison to assess the effect of postmenstrual age at time of scan on thalamic volume, as well as its effect on DTI parameters such as FA, MD, RD, and AD. Because the results of the DTI parameters showed similar patterns and radial diffusivity (RD) can capture decreased myelination better than FA, MD, or AD, we only chose to report RD changes.
We also assessed whether thalamic volume correlated with cortical thickness to understand their reciprocal growth. GLMs were used to test covariance between thalamic volume and vertex-wise cortical thickness while accounting for GA at birth.
Results
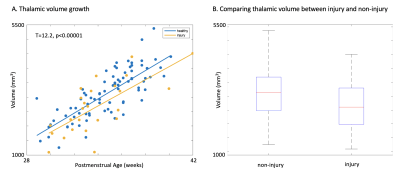
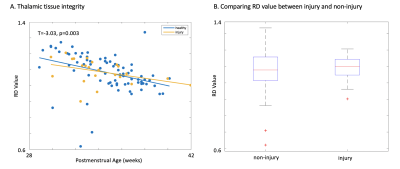
We found a positive correlation between age and thalamic volume (T=12, p<0.00001; Figure 1a). However, when accounting for mean group differences between injury and non-injury groups, no significant difference was found (p=0.003; Figure 1b).While we found a significant negative correlation between RD values and age, indicating intrathalamic myelination, no significant mean difference was found between injury and non-injury cohorts (Figure 2).
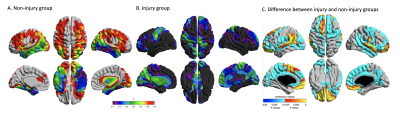
In the non-injury group, we found a significant correlation between thalamic volume and cortical thickness broadly in all cortical regions except the temporal lobe and part of the occipital lobe (Figure 3a). However, in the injury group, correlation between thalamic volume and cortical thickness markedly decreased (Figure 3b). The analysis of the interaction between the thalamocortical covariance and age at scan showed that the significantly decreased correlation in the injury group include a broad area of the cortex except the basal/medial temporal, middle frontal and superior parietal cortices.
Discussion and Conclusion
Our results suggest that prematurity-related injuries do not play a major role in thalamic growth and its myeloarchitecture. However, the covariance analysis show that injury may play a substantial role in thalamocortical maturational connectivity. The covariance between thalamic growth and cortical thickness significantly decreased with injury, suggesting that the perithalamic brain injury disrupts the hypothetic reciprocal signaling for the maturation of these two structures. In this context, this study leads to a better understanding of how prematurity-related injuries affect postnatal brain development, which may help clarify the underlying link between prematurity and adverse neurodevelopmental outcome in preterm survivors. To further clarify thalamocortical structural connectivity, however, DTI tractography is required in the future study.Acknowledgements
No acknowledgement found.References
1. Blakemore, C. and Z. Molnar, Factors involved in the establishment of specific interconnections between thalamus and cerebral cortex. Cold Spring Harb Symp Quant Biol, 1990. 55: p. 491-504.
2. Kelly, C.J., et al., Advances in neonatal MRI of the brain: from research to practice. Arch Dis Child Educ Pract Ed, 2019. 104(2): p. 106-110.
3. Wang, H.Z., et al., Multi-Atlas Segmentation with Joint Label Fusion. Ieee Transactions on Pattern Analysis and Machine Intelligence, 2013. 35(3): p. 611-623.
Figures