0209
Total loss of “swallow tail sign”: a potential substitute of PET for detecting dopaminergic degeneration in early-stage Parkinson’s disease1Fudan university Huashan hospital, Shanghai, China, 2Huashan Hospital, Fudan University,, Shanghai, China
Synopsis
Whether swallow tail sign (STS) could serve as a substitute or complement for nuclear medical imaging remains unclear. In this study, we compared STS features on MRI with striatal uptake on positron emission tomography (PET) at per nuclei level, construct an evaluation scale based on bilateral STS changes at the patient level, and estimate the diagnostic performance of the scale in 39 early-stage PD and 28 healthy controls. STS alterations corresponded well with striatal uptake on PET in early-stage PD. Total loss of STS is a reliable sign of nigrostriatal dopaminergic degeneration and might be a potential substitute for PET.
Introduction
Swallow tail sign (STS) is presumed to be an imaging biomarker of nigrosome-1 that can predict dopaminergic change in Parkinson’s disease (PD). However, whether it could serve as a substitute or complement for nuclear medical imaging remains unclear. Here, we compare STS features on MRI with striatal uptake on positron emission tomography (PET) at per nuclei level, construct an evaluation scale based on bilateral STS changes at the patient level, and estimate its diagnostic performance in early-stage PD.Methods
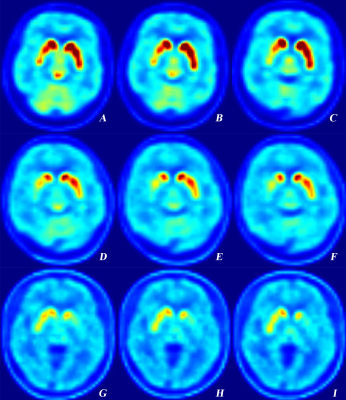
Thirty-nine patients with early-stage PD and 28 healthy controls (HCs) underwent quantitative susceptibility mapping (QSM) scanning on 3T MRI. Thirty-five of these patients were also assessed with [18F]9-fluoropropyl-(+)-dihydrotetra-benazine (18F-DTBZ) PET. Alterations of STS and striatal uptake in each hemisphere were visually rated on a 0-2 point scale (Fig.1 and 2). Concordance rate was calculated at nuclei level. The distribution of bilateral rating points between STS and striatal uptake was compared using Hotelling’s T-squared test. At participant level, an evaluation scale was acquired by adding bilateral STS points. Diagnostic power for PD was estimated using receiver operating characteristic analysis.Results
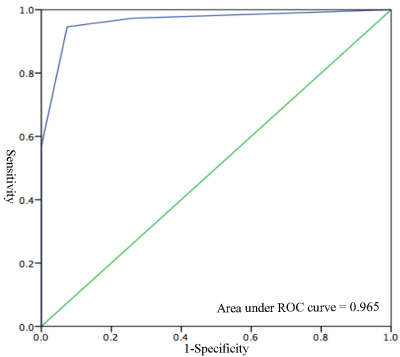
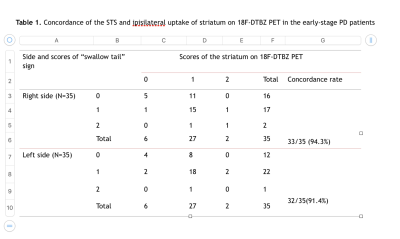
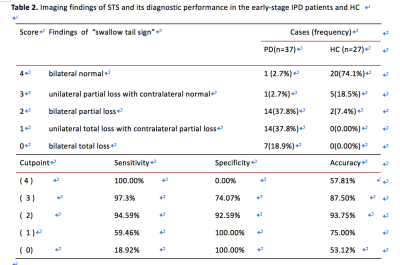
concordance of STS rating and ipsilateral striatal binding was 94.3% for the right side and 91.4% for the left (Table1.).From 70 total nuclei, 28 STS showed total loss with all of the ipsilateral striatum exhibiting decreased uptake; 39 STS displayed partial loss with 36 ipsilateral striatum presenting decreased uptake. The distribution of rating points showed no significant difference between the two imaging modalities. The evaluation scale revealed 36 out of 37 patients with abnormal STS. Bilateral total loss was observed in 7 patients, unilateral total loss with contralateral partial loss in 14 patients, bilateral partial loss in 14 patients, unilateral partial loss with normal contralateral in 1 patient (Table 2.). Using bilateral partial loss of STS as the threshold, achieved sensitivity and specificity for discriminating PD from HC were 94.59% and 92.49%, respectively (Table 2. and Fig. 3). Specificity was 100% when there was total loss of STS in one hemisphere.Conclusions
STS alterations corresponded well with striatal uptake on PET in early-stage PD. The evaluation scale of STS change used here has satisfactory diagnostic performance in discriminating the disease. Total loss of STS is a reliable sign of nigrostriatal dopaminergic degeneration and might be a potential substitute for PET.Acknowledgements
We are grateful to Dr.Kristina Zeljic for proofreading the manuscript. The study is supported by National Natural Science Fundation of China(NSFC61672236).References
1.Bae YJ, Kim JM, Kim E, et al. Loss of Nigral Hyperintensity on 3 Tesla MRI of Parkinsonism: Comparison With 123 I-FP-CIT SPECT. Mov Disord 2016;31(5):684-692.
2.Calloni SF, Conte G, Sbaraini S, et al. Multiparametric MR imaging of Parkinsonisms at 3 tesla: Its role in the differentiation of idiopathic Parkinson’s disease versus atypical Parkinsonian disorders. Eur J Radiol 2018;109(8):95-100.
3.Bae YJ, Kim JM, Kim KJ, et al. Loss of Substantia Nigra Hyperintensity at 3.0-T MR Imaging in Idiopathic REM Sleep Behavior Disorder: Comparison with 123 I-FP-CIT SPECT. Radiology 2018;287(1):285-293.
4. Mahlknecht P, Krismer F, Poewe W, Seppi K. Meta-analysis of dorsolateral nigral hyperintensity on magnetic resonance imaging as a marker for Parkinson's disease. Mov Disord 2017;32 (4):619-623.
Figures