0150
MRI-guided real-time 4D Radiation Dosimetry at an MRI-Linac using Polymer Gel Dosimeters1Engineering, Macquarie University, North Ryde - Sydney, Australia, 2Macquarie University, North Ryde - Sydney, Australia, 3Ingham Institute, Liverpool, Australia, 4The University of Sydney, Sydney, Australia
Synopsis
4D radiation dosimetry using a highly radiation-sensitive polymer gel dosimeter with real-time quantitative MRI readout is presented as a technique to acquire the accumulated radiation dose distribution during image guided radiotherapy (IGRT) in an MRI-Linac. Optimized T2 weighted TSE scans are converted to quantitative R2 maps and subsequently to radiation dose maps. A further increase in temporal resolution using a keyhole imaging approach is proposed. The potential use of real-time 4D radiation dosimetry for safeguarding image guided radiotherapy (IGRT) of moving and deforming targets in an MRI-Linac will be discussed.
INTRODUCTION
Image guided radiotherapy (IGRT) involves the application of real-time imaging during radiation where the motion of a tumour is tracked during radiation delivery. Feedback of the recorded tumour motion to the linear accelerator (Linac) enables synchronized delivery of radiation beams on the moving tumour volume. Recently, theragnostic MRI-Linac systems have been put in use that enable real-time MRI-guided tumour tracking during radiotherapy. The 4D nature of IGRT makes it difficult to assess the overall accuracy of the treatment. Indeed, a dephasing of the tumour motion with the moving treatment beam can cause more harm than a radiation delivery that does not accommodate for tumour motion. 4D dose verification is crucial in safeguarding IGRT delivered with an MRI-Linac.We hereby present the first results of real-time MRI on a radiation-sensitive polymer gel dosimeter (PGD) during radiation delivery on the Australian MRI-Linac. PGDs consist of hydrogels in which acrylic monomers are dispersed. Upon exposure to ionizing radiation, a radiation-induced polymerization reaction occurs. The created polymer is fixated by the hydrogel matrix. Anthropomorphic shaped PGDs have been applied successfully to capture the radiation dose distribution in three dimensions delivered during radiotherapy (RT) 1. In this study, real-time radiation dosimetry in MRI guided radiotherapy is illustrated while a further increase in readout speed is aimed with keyhole MRI.
METHODS
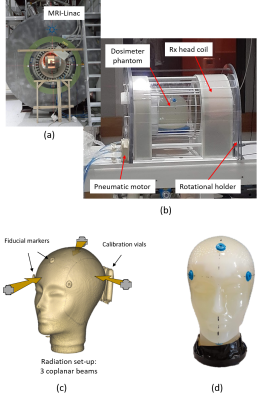
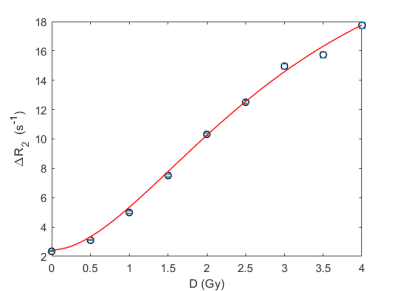
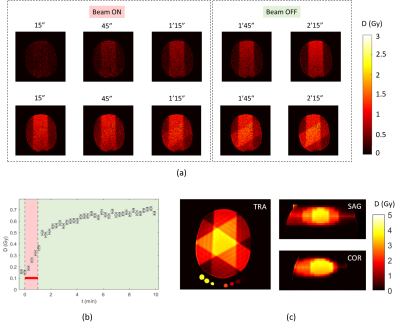
PGDs based on 6%(wt) methacrylic acid and 8%(wt) gelatin, referred to as MAGAT, were fabricated according to a recipe discussed elsewhere 2. MRI scanning and radiation of the PGDs was performed on the 1T Australian MRI-Linac (Figure 1a). The PGDs were also scanned 26 hours post-radiation on a clinical 3T MRI (Siemens Verio). Calibration PGD vials were irradiated in a standard water phantom at reference depth (10 cm) at a dose rate of 1 Gy/min. A head shaped PGD was irradiated with 3 coplanar beams (Figure 1c) at similar dose rates. An in house fabricated pneumatic driven automated rotational holder was used to rotate the gel dosimeter in between consecutive radiation beams inside the head coil (Figure 1b).The PGDs were scanned dynamically during radiation exposure inside the receive head coil with a T2-weighted (T2w) Turbo-Spin Echo (TSE) sequence (TE/TR/TurboFactor/BWpix/FOV/MS/slice thickness = 147ms/1s/13/130Hz/200mm/192x192/5mm), resulting in a temporal resolution of 15 s/scan. After radiation delivery, the head phantom dosimeter and calibration vials were scanned together with a Multi-Spin-Echo (MSE) sequence with 32 echoes (echo time spacing: 15 ms) from which a calibration curve was obtained that relates the $$$R_2$$$ value ($$$R_2 = \frac{1}{T_2}$$$) with the absorbed radiation dose $$$D$$$. The dynamic scans were converted to $$$\triangle R_2$$$ maps by applying the equation $$$\triangle R_2(t) = \frac{1}{TE} ln(\frac{S(t)}{S(0)})$$$ where $$$S(t)$$$ is the T2w pixel intensity acquired at a radiation time $$$t$$$ and $$$S(0)$$$ is the T2w pixel intensity before radiation. The dose $$$D$$$ is obtained by applying a calibration plot $$$D(\triangle R_2)$$$ that is extracted from a bi-exponential fit on the irradiated calibration vials.
RESULTS
The R2-dose calibration plot of the MAGAT PGD was found to follow a sigmoid shape (Figure 2). A small increase in R2-dose sensitivity was found 26 hours after radiation which is attributed to post-radiation polymerization 2. The R2-dose-sensitivity in the dose range [1Gy, 2Gy] was found to be 4.9 s-1.Gy-1 immediately after radiation and 5.5 s-1.Gy-1 26 hours post-radiation, which is the highest sensitivity ever registered in PGDs 2,3. The registered dose was found to increase linearly during radiation (Figure 3a-b), followed by a smaller increase immediately after radiation indicating ongoing polymerization.During dynamic scanning, measurable changes in dose were visible between two imaged frames. Inter-leaf radiation leakage (in the order of 13%) is clearly visible on dose maps obtained from quantitative R2 scans in the central plane where leaf-banks of the multi-leaf collimator are touching (Figure 3c).
DISCUSSION
To enable real-time 4D radiation dosimetry in a gel dosimeter, a high radiation-induced chemical conversion rate is required in combination with a large change in MRI contrast. In addition, the radio-chemical reaction needs to be fast enough to cause a measurable change in MRI contrast between subsequent scanning time frames. First experiments with Fricke gel dosimeters (results not shown) demonstrated a too low sensitivity (0.01 s-1.Gy-1) to be useful for 4D radiation dosimetry. The R2-dose sensitivity of MAGAT PGD is about 500 times higher than that of a Fricke gel dosimeter. T1, T2, magnetization transfer and chemical shift were investigated as potential contrast mechanisms for both dosimeters. T2 contrast was found to result in the highest contrast yield per radiation unit.For the current experiments, a TSE sequence with fixed effective echo time was used to acquire dynamic frames with a temporal resolution of 15 s. It can be shown that the theoretical optimal echo time ($$${TE}_{opt}$$$) to achieve maximum interframe signal contrast is inversely related to the R2 at any moment in time (i.e. $$${TE}_{opt} = \frac{1}{R_2}$$$). To further increase the temporal resolution, a keyhole approach with a single shot TSE readout per frame is proposed.
CONCLUSION
Real-time 4D radiation dosimetry using high-sensitive PGDs with inline MRI readout on an MRI-Linac has been demonstrated. Further research is focussed on faster quantitative readout methods that will enable 4D radiation dosimetry with higher radiation dose rates.Acknowledgements
References
1. De Deene Y, De Wagter C, Van Duyse B, et al. Validation of MR-Based Polymer Gel Dosimetry as a Preclinical Three-Dimensional Verification Tool in Conformal Radiotherapy, Magn Reson Med. 2000, 43:116-125.
2. De Deene Y, Vergote K, Claeys C, et al. The fundamental radiation properties of normoxic polymer gel dosimeters: a comparison between a methacrylic acid based gel and acrylamide based gels, Phys Med Biol. 2006, 51: 653-73.
3. Baldock C, De Deene Y, Doran S, et al. Polymer gel dosimetry, Phys Med Biol. 2010, 55: R1-R63.
Figures