0118
To assess and follow-up the mpMRI and prostate volumetric changes after whole prostate MR-guided transurethral prostate ultrasound ablation.
Afshin Azadikhah1, Holden Wu2, Melina Hosseiny2, and Steven S Raman2
1Radiology, University of California, Los Angeles, Los Angeles, CA, United States, 2University of California, Los Angeles, Los Angeles, CA, United States
1Radiology, University of California, Los Angeles, Los Angeles, CA, United States, 2University of California, Los Angeles, Los Angeles, CA, United States
Synopsis
To evaluate the changes of 3 Tesla (3T) mpMRI and PSA parameters before and during multiple time points after whole gland prostate cancer (PCa) treatment using MRI-guided directional transurethral ultrasound ablation (TULSA). Patients were treated and followed-up for 1, 3, 6 and 12-month in retrospective, cohort, a trial study from October 2017 to February 2019. The mean ADC value, T2W, NPV, PSAD, and prostate volume were significantly decreased after 1 to 12-month follow-up with significant differences. MRI-guided TULSA uses a minimally-invasive transurethral approach, and this appears to be an effective method especially in patients with localized, organ-confined prostate cancer.
Introduction
Traditional whole gland treatment for prostate cancer is complicated by urinary incontinence and erectile dysfunction in up to 30-50% of the patients(1, 2). MR Guided Transurethral US has been previously shown to be safe and effective for whole gland prostate ablation for patients with prostate cancer and might be a novel whole gland ablation technique. However, prostatectomy remains the standard of treatment for patients with more aggressive disease. But, a significant number of patients have other comorbidities, making them not good candidates for surgery. This study aims to evaluate the safety and efficacy of whole gland MRI-guided transurethral ultrasound ablation (TULSA) for prostate cancer treatment in patients with low-intermediate grade prostate cancer.Methods
This IRB approved, HIPAA compliant study included 9 men (45 to 80 years) with biopsy-confirmed PCa, clinical-stage <T2b, Gleason score (GS) ≤ 3+4, PSA ≤ 15 ng/ml and prostate volume ≤ 90 cc. The whole prostate was ablated with 3T MRI guided TULSA along with a rectal cooling probe. Patients were followed-up (F/U) at 1, 3, 6, and 12 months after the treatment with measurements of PSA and 3T mpMRI. The prostate non-perfused volume (NPV) was measured on contrast-enhanced T1-weighted images at each F/U. A paired T-test was used to compare each subject's pre-treatment measurements to their last value F/U measurement (p<0.05 considered significant). TRUS-guided 10-core prostate biopsy was performed 12 months after ablation.Results
In 17 PCa lesions from 9 patients, 8 were GS 3+3, and 9 were 3+4. The mean prostate ablation time was 89 min. (range 30-120 min). All of the cases were clear of the lesion on biopsy 12 months after treatment. There were no immediate intra-procedural or post-procedural complications. Mean prostate volume on T2-weighted MRI decreased from 46cc at baseline to 32cc (29%), 24cc (49%), 21cc (54%) and 13cc (70%) on 3, 6, & 12-month F/U, respectively (p=0.01). The mean prostate NPV decreased from 33.7cc (range 13-83cc) to 21cc (38.3%), 15cc (56.6%), 11cc (68.8%) and 2cc (94.2%) on 1, 3, 6, and 12-month F/U, respectively. Mean PSA density (PSAD) decreased from 0.19 ng/ml2 before treatment to 0.02 on 1-month F/U and then increased gradually to 0.09, 0.15 and 0.06 at 3, 6 and 12-month F/U, respectively. The mean ADC value decreased 7.4% from 1460 mm-6/s2 ± 117 at baseline to 1351 mm-6/s2 ± 130 on the 12-month F/U (p=0.079). The mean T2W decreased 61.9% from 374 ms ± 261 at baseline to 143 ms ± 73 on the 12-months F/U (p=0.052). The mean T1-weighted contrast decreased by 22.2% from 427 ms ± 312 at baseline to 332 ± 81 on the 12-month F/U (p=0.378).Discussion
In this study, we have found that MR guided transurethral ultrasound was safe and resulted in a significant decrease in prostate volume at 1, 3, 6, and 12 months with a corresponding significant decrease in PSAD, NPV, and PSA. In Bonekamp et al study, 88% reduction in prostate volume at 12 months F/U was reported similar to our study. Moreover, ADC decreased in the post ablated prostate, as shown in prior studies. Jakob et al(3) reported decreases in post-treatment ADC values for non-treated fibroid tissue (1685mm-6/sec2 ± 468) compared to post-treatment ADC values for fibroid tissue (1078 mm-6/sec2 ± 293) (p=0.001). T2-weighted imaging is susceptible to differences in the area of the magnetic domain and is helpful for considering ablated texture(4). Wang et al(5) have reported that average T2 (57.8 msec ± 25.3) in the pre-ablation area was significantly higher than T2 (38.9 msec ± 14.1) in the same area after treatment (P=0.03). Westin et al(6) also reported increases in T2 values in areas of ablation from (94.99 msec ± 25.07) at the baseline to (93.41 msec ± 35.19) 3 months after ablation and, (105.27 msec ± 63.67) 12 months after treatment.Conclusions
In conclusion, the new MRI-guided TULSA procedure treated the whole prostate gland in an outpatient setting without significant complications in patients with low-intermediate grade PCa, with a significant, the predictable decrease in prostate volume and PSA density, and with considerable changes in mpMRI parameters at multiple F/U time points.Acknowledgements
No acknowledgement found.References
1. Ghai S, Perlis N, Lindner U, Hlasny E, Haider MA, Finelli A, Zlotta AR, Kulkarni GS, van der Kwast TH, McCluskey SA, Kucharczyk W, Trachtenberg J. Magnetic resonance guided focused high frequency ultrasound ablation for focal therapy in prostate cancer - phase 1 trial. Eur Radiol 2018;28(10):4281-4287. doi: 10.1007/s00330-018-5409-z 2. Zambon JP, Patel M, Hemal A, Badlani G, Andersson KE, Magalhaes RS, Lankford S, Dean A, Williams JK. Nonhuman primate model of persistent erectile and urinary dysfunction following radical prostatectomy: Feasibility of minimally invasive therapy. Neurourol Urodyn 2018;37(7):2141-2150. doi: 10.1002/nau.23536 3. Jacobs MA, Herskovits EH, Kim HS. Uterine fibroids: diffusion-weighted MR imaging for monitoring therapy with focused ultrasound surgery--preliminary study. Radiology 2005;236(1):196-203. doi: 10.1148/radiol.2361040312 4. Foxley S, Domowicz M, Karczmar GS, Schwartz N. 3D high spectral and spatial resolution imaging of ex vivo mouse brain. Med Phys 2015;42(3):1463-1472. doi: 10.1118/1.4908203 5. Wang S, Fan X, Yousuf A, Eggener SE, Karczmar G, Oto A. Evaluation of Focal Laser Ablation of Prostate Cancer Using High Spectral and Spatial Resolution Imaging: A Pilot Study. J Magn Reson Imaging 2018. doi: 10.1002/jmri.26538 6. Westin C, Chatterjee A, Ku E, Yousuf A, Wang S, Thomas S, Fan X, Eggener S, Karczmar G, Oto A. MRI Findings After MRI-Guided Focal Laser Ablation of Prostate Cancer. AJR Am J Roentgenol 2018;211(3):595-604. doi: 10.2214/ajr.17.19201Figures

Changes
in NPV at each
follow-up.
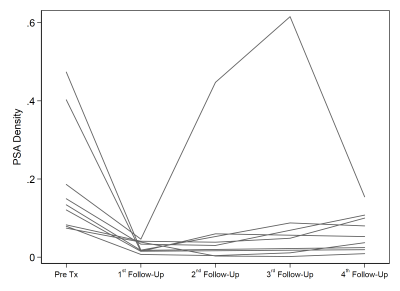
The
68.4% difference between mean PSAD=0.19 at baseline and 0.06 at 12 months was
significant (p=0.041).
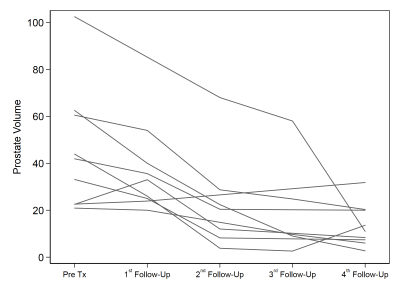
Changes
in Prostate Volume at each
follow-up
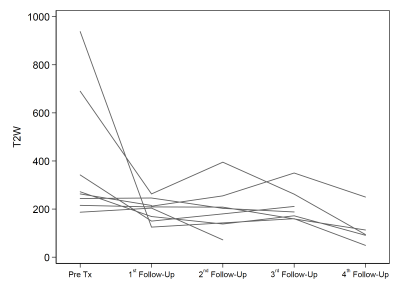
The mean T2-weighted decreased 61.9% from
374 ms± 261
at baseline to 143 ms ± 73 at 12 months F/U (p=0.052).
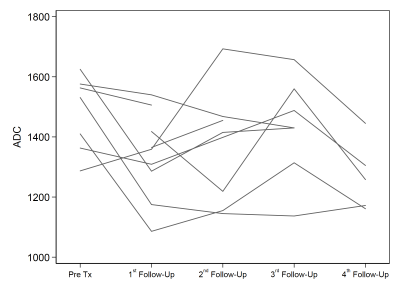
changes in ADC at each time point with significant changes.