0075
MR imaging and MR guided biopsy in initial diagnosis and staging of pediatric malignancies – a one-stop shop approach1Diagnostic and Interventional Radiology, Saarland University Medical Center, Homburg, Germany
Synopsis
Diagnosis and staging in pediatric malignancies today involves different imaging procedures, from conventional x-ray over ultrasound to MR-, CT- and PET-imaging. We evaluated as if MRI can be used as a comprehensive one-stop shop for diagnosis, staging and biopsy in pediatric malignancies. As a result, when comparing the different imaging modalities, differences between MRI and CT were seen regarding the higher number of small lung lesions detected (<3mm) on CT. Comparable results were seen for abdominal tumors, Hodgkin- and Non-Hodgkin Lymphoma. In Ewing sarcoma MRI showed advantages compared with PET imaging regarding detection of skip lesions and bone marrow metastases.
PURPOSE
Diagnosis and staging of pediatric malignancies nowadays involves a variety of imaging procedures, from conventional x-ray and ultrasound to MRI, CT and PET imaging 1-5.The aim of our study was to determine whether MRI can be used as a comprehensive one-stop shop procedure for diagnosis, staging and biopsy of pediatric malignancies.To overcome the problems of intubation and controlled ventilation for dynamic T1w CE imaging of the thorax and abdomen in MRI, imaging for staging as well as MR-guided biopsy was performed on a 3T magnet (Siemens Magnetom Vida) applying non-breathhold techniques.
METHODS AND MATERIALS
Twenty-six patients aged from 2 weeks to 12 years were evaluated on a 3 T scanner (Siemens, Magnetom VIDA). Overall, 21 whole body MR examinations and 5 studies of thorax, abdomen and pelvis were performed. All patients underwent MRI under sedation with free breathing, applying non-breathhold techniques. Images were acquired using T2w radial and respiratory gated sequences, T1w dynamic GRASP sequences, static T1w radial VIBE sequences applying Dixon fat suppression pre- and post-contrast as well as diffusion weighted (DWI) sequences. DWI was acquired during free breathing and transversal T2w-TSE sequences and a composed coronal whole-body STIR-sequence completed the whole-body imaging approach. For patients with bone tumors sequences to allow for local staging were performed in addition to whole body imaging. For patients with abdominal and thoracic tumors T1w images were acquired from neck to pelvis both pre-contrast and post-contrast after injection of 0.05 mmol/kg BW MultiHance if liver imaging was planned or 0.1 mmol/kg ProHance. For MR-guided biopsies a HASTE sequence was used during positioning of the biopsy needle, to allow for fast high contrast imaging. MRI was performed prior to other staging procedures and diagnosis based on MR-imaging was performed without knowledge of the results of other imaging modalities performed subsequently. To evaluate the performance of MRI, the MRI reports were compared to findings from established staging procedures including PET, MIBG or bone scintigraphy, CT and ultrasound. When available histology was considered the reference standard diagnosis. In the absence of histology findings final diagnosis was based on the results of the established imaging techniques if there was discordance with those of MRI.RESULTS
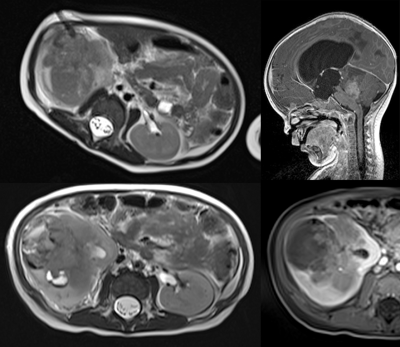
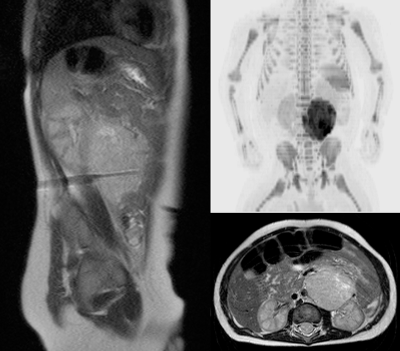
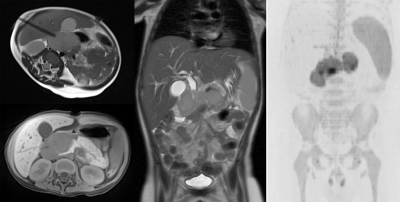
The final diagnoses of the 26 patients evaluated were lymphoma (n=8), different types of bone and soft tissue sarcoma (n=7) and solid tumors including neuro-, nephro- and hepatoblastoma, rhabdoid tumors and germ cell tumors (n=11). Tissue samples to acquire histologic confirmation, including genetic testing, was obtained from MR-guided biopsy of tumors or metastases in 18 out of 26 patients. In cases of neuroblastoma, tissue biopsies allowed for evaluation of n-myc amplification6. In the remaining 8 patients, laboratory findings, typical imaging appearance or bone marrow samples allowed for diagnosis.When comparing the different imaging modalities, an advantage for CT over MRI was seen only for the detection of small (<3 mm) lung metastases, however these differences did not result in a change of patient management. For abdominal tumors, MRI using high resolution non-breath-hold dynamic CE imaging was able to detect small liver metastases not seen on CT, MIBG scinitigraphy or PET imaging. Comparable results were seen for whole-body MRI of Hodgkin-, Non-Hodgkin and T-cell Lymphoma, in which MRI demonstrated a similar extent of disease to that seen on PET-imaging. Minor differences involved small, PET positive lymph nodes, however histologic proof was not available in most of these cases.In patients with Ewing sarcoma, MRI showed advantages over PET imaging for detection of skip lesions and bone marrow metastases. In these cases of Ewing sarcoma, histologic proof was achieved and the additional findings in MRI resulted in a change of patient management.CONCLUSION
Whole body MRI can correctly stage and diagnose a variety of malignant tumors in pediatric patients and allows for accurate patient management including MR-guided biopsy. Advantages of established imaging methods were seen only for detection of small lung metastases on pulmonary CT. However, the detected addition lung lesions could not be classified as benign or malignant based on CT imaging findings and the only consequence was a follow-up study. In all other cases, MRI could serve as a one-stop shop for the diagnosis and staging of malignant tumors in pediatric patients. Further studies have to evaluate, if MRI can also serve as a technique to evaluate tumor response to therapy, an area where today especially in Hodgkin- and non-Hodgkin lymphoma PET imaging is the gold standard.Acknowledgements
The authors want to thank all colleagues from the department of pediatric oncology for there help in this study.References
1. Swift CC, Eklund MJ, Kraveka JM et al. Updates in Diagnosis, Management, and Treatment of Neuroblastoma. Radiographics. 2018 Mar-Apr;38(2):566-580
2. Guimarães MD, Noschang J, Teixeira SR et al. Whole-body MRI in pediatric patients with cancer. Cancer Imaging. 2017 Feb 10;17(1):6
3. Eutsler EP, Khanna G. Whole-body magnetic resonance imaging in children: technique and clinical applications. Pediatr Radiol. 2016 May;46(6):858-72
4. Servaes SE, Hoffer FA, Smith EA et al. Imaging of Wilms tumor: an update. Pediatr Radiol. 2019 Oct;49(11):1441-1452
5. McCarten KM, Nadel HR, Shulkin BL et al. Imaging for diagnosis, staging and response assessment of Hodgkin lymphoma and non-Hodgkin lymphoma. Pediatr Radiol. 2019 Oct;49(11):1545-1564
6. Berbegall AP, Bogen D, Pötschger U et al. Heterogeneous MYCN amplification in neuroblastoma: a SIOP Europe Neuroblastoma Study. Br J Cancer. 2018 May;118(11):1502-1512
Figures
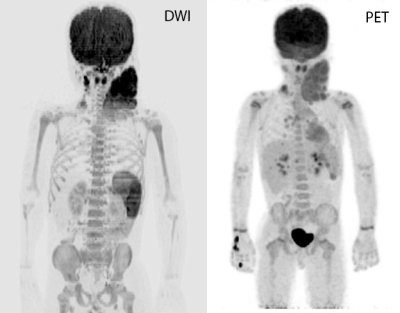
MIP projection of diffusion weighted imaging (left) and PET imaging (right) in a patient with Hodgkin disease.
DWI and PET imaging show almost perfect correlation.