0074
3D PDWI Accelerated with Compressed SENSE in Pediatric Joint Imaging: Clinical Feasibility Study1Department of Radiology, Beijing Children’s Hospital, Capital Medical University, National Center for Children's Health, Beijing, China, 2Philips Healthcare, Beijing, China
Synopsis
The use of three dimensional (3D) volumetric acquisition in clinical settings has been limited due to long scan time. However, 3D volumetric acquisition could provide higher spatial resolution and decrease partial volume effects. The introduction of compressed sensing in combination of the parallel imaging technique SENSE allows shortening of scan time and provide comparable overall image quality when compared with standard sequences. The purpose of the study is to determine the feasibility of 3D PDWI accelerated with compressed SENSE(CS) for evaluating the pediatric joint image quality and compared with 2D PDWI.
Introduction
The use of three dimensional (3D) volumetric acquisition in clinical settings has been limited due to long scan time. However, 3D volumetric acquisition could provide higher spatial resolution and decrease partial volume effects. The introduction of compressed sensing in combination of the parallel imaging technique SENSE1-3 allows shortening of scan time and provide comparable overall image quality when compared with standard sequences. The purpose of the study is to determine the feasibility of 3D PDWI accelerated with compressed SENSE1-3 (CS) for evaluating the pediatric joint image quality and compared with 2D PDWI.Materials and Methods
Twenty pediatric patients (age, 1 to 10 years old) for joint examinations were performed on a 3.0T MR scanner (Ingenia CX, Philips Healthcare, the Netherlands) using knee and hip coils. The protocol consisted of 2D sagittal proton density weighted image (2D-PDWI) and 3D PDWI accelerated with CS (3D-PDWI-CS). Signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR, between bone and muscle) of 3D-PDWI-CS were compared with those of 2D-PDWI. Image quality of two sequences was analyzed by two readers independently, who were blinded to any clinical information (5 years of experience in MR imaging and 10 years of experience in MR imaging). Subsequently, a final interpretation was made in consensus. A third experienced radiologist (15 years of experience in MR imaging) involved in case of disagreements. Image quality of both sequences for each patient was rated according to a 5-point Likert scale (score of 1, nondiagnostic; score of 2, poor; score of 3, moderate; score of 4, good; and score of 5, excellent). The main evaluation indexes include the following: 1) patients with normal joint: articular cartilage and bone cortex, bone trabecula, muscle texture and boundary, fine details of anatomic structures, noise and artifacts, and overall image quality. 2) patients with abnormal joint: lesion location, contrast of lesions, muscle injury boundary and contrast between lesions and surrounding tissue.4 Image quality was measured by the quantitative and qualitative methods described above. The paired t-test or a Wilcoxon rank analyses were performed between 2D-PDWI and 3D-PDWI-CS. Interobserver agreement for the qualitative evaluation of image quality was calculated using weighted kappa analysis, and weighted kappa analysis for ordinal variables including the five-point visual scoring systems. P values< 0.05 were considered significant.3Results
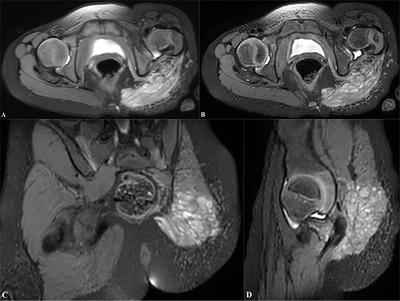
The bone SNR (26.45±13.65 vs. 26.87±11.86; P>0.05) and muscle SNR (34.79±17.94 vs. 34.65±10.28; P>0.05) showed no statistical significant different between 2D-PDWI and 3D-PDWI-CS. The joint CNR between bone and muscle (8.97±7.83 vs. 10.42±6.51; P>0.05) showed no statistical significant between 2D-PDWI and 3D-PDWI-CS. Compared with 2D-PDWI, more imaging anatomical details were clearly shown at 3D-PDWI-CS at the double scan time. At the double scan time, articular cartilage and bone cortex, bone trabecula and muscle texture and boundary were clearly shown on the sagittal images at 3D-PDWI-CS. The more details of lesion location, contrast of lesions, muscle injury boundary and contrast between lesions and surrounding tissue were shown at 3D-PDWI-CS. Although the contrast of the original image was better, the image contrast of reformatted image from 3D-PDWI-CS was poorer than that of 2D-PDWI, especially on the display of lesions. The two observers showed moderate and good interobserver agreement on the five-point visual scoring system for 2D-PDWI and 3D-PDWI-CS respectively (weighted kappa, 0.508 and 0.681 respectively. p<0.05).Conclusions
3D-PDWI-CS outperforms conventional 2D-PDWI sequence in pediatric joint MR imaging as scan times doubling changed while image quality is maintained or even improved. Although the scan time of a single sequence is longer, the overall inspection time is shorter. 3D-PDWI-CS is a reliable alternative for clinical use in pediatric joint MR imaging. Although reformatted image contrast is poor, 3D-PDWI-CS can provide higher resolution with less partial volume effect, multi-directional image reformat, and further image analysis.Acknowledgements
No acknowledgement found.References
[1] Sartoretti T, Sartoretti E, Wyss M, et al. Compressed SENSE accelerated 3D T1w black blood turbo spin echo versus 2D T1w turbo spin echo sequence in pituitary magnetic resonance imaging. Eur J Radiol 2019; 120:108667.
[2] Nam JG, Lee JM, Lee SM, et al. High Acceleration Three-Dimensional T1-Weighted Dual Echo Dixon Hepatobiliary Phase Imaging Using Compressed Sensing-Sensitivity Encoding: Comparison of Image Quality and Solid Lesion Detectability with the Standard T1-Weighted Sequence. Korean J Radiol 2019;20(3):438-448.
[3] Cho SJ, Choi YJ, Chung SR, et al. High-resolution MRI using compressed sensing-sensitivity encoding (CS-SENSE) for patients with suspected neurovascular compression syndrome: comparison with the conventional SENSE parallel acquisition technique. Clin Radiol 2019;74:817.e9-817.e14.
[4] Wintersperger BJ, Runge VM, Biswas J, et al. Brain tumor enhancement in MR imaging at 3 Tesla: comparison of SNR and CNR gain using TSE and GRE techniques. Invest Radiol 2007;42(8):558-563.
Figures

SPAIR= spectral attenuated inversion recovery
SNR1=SNR of bone, SNR2=SNR of muscle, ROI=28mm2, CNR=between bone and muscle
The weighted kappa was categorized as follows: <0.20, poor;0.21~0.40, fair; 0.41~0.60, moderate; 0.61~0.80, good; 0.81~1.00, excellent.