0043
C5 level area can replace whole cervical spinal cord area measurements in multiple sclerosis as a practical biomarker of progression1Radiology, Mayo Clinic, Rochester, MN, United States, 2Neurology, Mayo Clinic, Rochester, MN, United States, 3Marmara University School of Medicine, Istanbul, Turkey, 4Viral Immunology Section, Neuroimmunology and Neurovirology Division, National Institute of Neurological Disorders and Stroke, Bethesda, MD, United States, 5Translational Neuroradiology Section, Neuroimmunology and Neurovirology Division, National Institute of Neurological Disorders and Stroke, Bethesda, MD, United States
Synopsis
Subclinical progression reflecting neurodegeneration can be measured and followed through spinal cord volume monitoring in multiple sclerosis (MS). The increased atrophy is reflected more prominently in the caudal cervical spinal cord segment. In this study, we identified the C5 level area measurement which can reflect whole cervical spinal cord area in patients with MS using both semi-automated and manual measurements. We propose that the C5 level area measurement can replace whole cervical spinal cord area measurement in MS as a more practical biomarker of progression.
Introduction
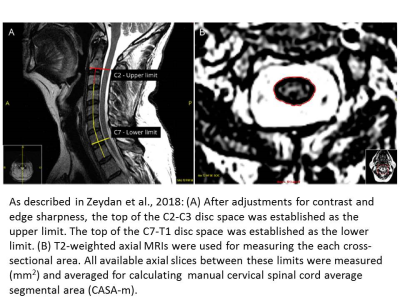
Cervical spinal cord atrophy is a biomarker that associates with disability worsening in MS.1 We have shown that cervical spinal cord atrophy marks the evolution from relapsing-remitting phase to progressive phase in MS.2 The study construct required the use of heterogeneously-sourced clinical MRIs, since the ultimate determination of PMS required retrospective time-point analyses. Therefore, we used a manual approach using cervical spinal cord area measurements at C2 and C7 levels as well as cervical spinal cord average segmental area (CASA-m) from C2 to C7 (Figure-1). All three areas were significantly smaller at the time of progressive MS (PMS) onset than age-matched individuals with radiologically isolated syndrome (pre-symptomatic MS). Caudally the area was smaller in patients with PMS than age-matched patients with relapsing-remitting MS without progression.2 At the time of PMS clinical manifestation, there was already loss of cervical spinal cord volume hinting at subclinical neurodegeneration that can be detected by spinal cord volume monitoring in MS. The cranio-caudal increase in cervical spinal cord volume loss in MS was recently independently confirmed in PMS.3 Semi-automated methods are widely used to measure cervical spinal cord atrophy, especially in clinical trials with research-standardized MRIs, while manual approach stands as the gold standard to develop such methods and for heterogeneously-sourced clinical MRIs may represent the right choice. In the current study, we aimed to identify a single cervical spinal cord area of the lower cervical cord segment to: 1) reflect the cranio-caudal pattern of increased atrophy in MS, and 2) sufficiently represent CASA, so that it could be utilized in both standardized and non-standardized serial MRIs.Methods
One hundred eighty two non-standardized cervical spinal cord MRIs from 63 individuals with MS (45 RRMS, 18 PMS; 46 women, 17 men) obtained during routine clinical visits were analyzed. We used two independently developed and previously published manual (test-retest agreement R>0.97) and semi-automated methods.2,4 Cervical spinal cord areas at individual levels cranio-caudally from C1/C2 to C7 were measured and averaged by two individuals (SU&TD) using the alternate methods blinded to each other’s measurements. In the manual approach, cross-sectional areas for each level (C2-C7) were measured twice by the same individual and averaged to calculate CASA-m (31 MRIs). In the semi-automated approach, T1-weighted sagittal images were used to measure each cross-sectional area (C1-C7) as well as CASA-sa (182 MRIs). We initially defined upper (C1/C2-C3), middle (C3-C5) and lower (C5-C7) cervical spinal cord segments and tested their correlations with CASA-m with the manual method. After identifying which segment correlated the best with CASA-m, we separately analyzed each individual cervical spinal cord level using the manual method. Next, we replicated the above analyses in the semi-automated method. After confirming C5 as the common cervical spinal cord level that correlated the best with CASA using both methods, we measured C5 area manually in additional 151 MRIs. Finally, we studied the correlations between age and C5 cervical spinal cord areas using both methods in 182 MRIs to show if age associated decline in spinal cord volume can be reflected in a single segment measurement.Results
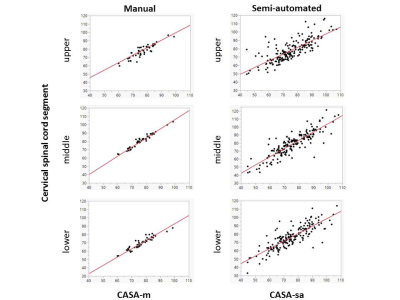
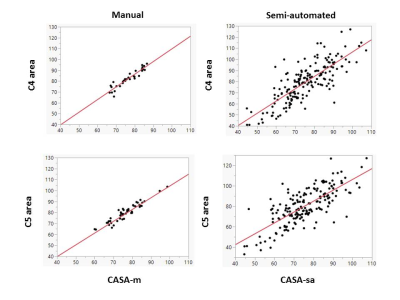
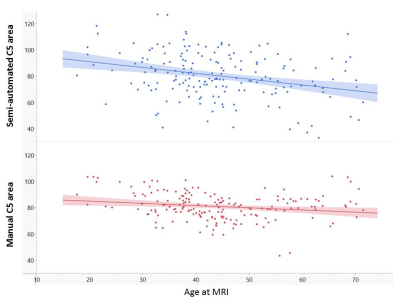
In the manual method, all cervical spinal cord segment areas (upper, middle and lower) correlated with CASA-m. The strongest correlation was between middle cervical spinal cord segment and CASA-m. (n=31; upper R=0.89, p<0.001; middle R=0.98, p<0.001; lower R=0.93, p<0.001) (Figure-2). Among all individual levels, C4 and C5 cervical spinal cord areas correlated the best with CASA-m (n=31; C4 area R=0.94, p<0.001; C5 area R=0.93, p<0.001) (Figure-3). In the semi-automated method, the strongest correlation was between lower cervical spinal cord segment and CASA-sa (n=182; upper R=0.73, p<0.001; middle R=0.80, p<0.001; lower R=0.83, p<0.001) (Figure-2). Consistent with our manual method results, C4 and C5 correlated the best with CASA-sa (n=182; C4 area R=0.79, p<0.001; C5 area R=0.75, p<0.001) (Figure-3). Eventually, C5 level was identified as the overlapping spinal cord level that captured the switch from middle to lower cervical spinal cord segments and correlated the best with CASA using both methods. Age and C5 area inversely correlated using both manual (R=‑0.19, p=0.0099) and semi-automated (R=‑0.30, p<0.0001) methods with indistinguishable slopes and variation from the mean (Figure-4).Discussion
We show that C5 level area measurement reflecting the cranio-caudal loss of spinal cord volume in MS could be utilized as a single level biomarker in MS. Recent studies indicate that such a direction is indeed practical3 for clinical trials both as a subclinical outcome measure and as a biomarker of future clinical evolution in MS. Cervical spinal cord atrophy is a biomarker of sub-clinical progression in MS that can potentially be utilized during the relapsing-remitting phase to make treatment escalation decisions currently, or if and when available introducing disease modifying medications to slow neurodegeneration in MS. Single segment measurements that can reflect what is gained by measuring the whole cervical spinal cord area could therefore greatly facilitate ease of application. We did not have thoracic cord scans which may also be relevant in reflecting the cranio-caudal pattern of atrophy in MS.4Conclusion
Single level area measurements especially at C5 level can practically be utilized to reflect average cervical spinal cord area in patients with MS.Acknowledgements
Funded by National Institute on Aging. (U54 AG 44170) - Career Enhancement Award to Dr. Zeydan.References
1. Lukas C, Knol DL, Sombekke MH, Bellenberg B, Hahn HK, Popescu V, et al. Cervical spinal cord volume loss is related to clinical disability progression in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2015;86(4):410-8.
2. Zeydan B, Gu X, Atkinson EJ, Keegan BM, Weinshenker BG, Tillema JM, et al. Cervical spinal cord atrophy: An early marker of progressive MS onset. Neurol Neuroimmunol Neuroinflamm. 2018;5(2):e435.
3. Rocca MA, Valsasina P, Meani A, Gobbi C, Zecca C, Rovira A, et al. Clinically relevant cranio-caudal patterns of cervical cord atrophy evolution in MS. Neurology. 2019.
4. Liu W, Nair G, Vuolo L, Bakshi A, Massoud R, Reich DS, et al. In vivo imaging of spinal cord atrophy in neuroinflammatory diseases. Ann Neurol. 2014;76(3):370-8.
Figures