RF Field Simulations & Safety Aspects
1Stanford University, United States
Synopsis
A major challenge that currently hinders the application of Ultra High-Field (UHF) MRI in clinical diagnostics is the non-uniform deposition of radiofrequency (RF) power in the body. Electromagnetic modeling has become a popular tool to assess SAR in simulation [10]-[14]. A diverse family of detailed body models can be used to estimate global SAR and peak local SAR. While SAR values can still vary from patient to patient, with patient position, and with other variables, these simulations provide a strong basis for novel approaches that tackle SAR prediction more accurately [15]-[17]. Given the strong incentive to develop UHF MRI into a clinical tool, it is paramount to find a viable and accurate method for monitoring the spatially varying SAR pattern, and therefore the actual ratio of peak local SAR to global SAR, as the key parameter in MRI safety.
Introduction
A major challenge that currently hinders the application of Ultra High-Field (UHF) MRI in clinical diagnostics is the non-uniform deposition of radiofrequency (RF) power in the body. This safety issue is one of the most important limiting factors in the design and use of the RF components for UHF MRI, since there is a risk of patient injury through the deposition of high RF power levels within small regions (“hotspots”) for extended times, leading to local heating with potential tissue damage. The key parameter used in characterizing MR safety for RF coils is the specific absorption rate (SAR), which measures the power delivered to a certain mass of tissue in W/kg. Current technology is not equipped to measure SAR locally; the only quantity that can be easily determined in-vivo is the overall average, or global, SAR, which is a measure of the average power absorbed per unit mass of tissue that is delivered to the entire mass of the body part under investigation (e.g. head or torso).
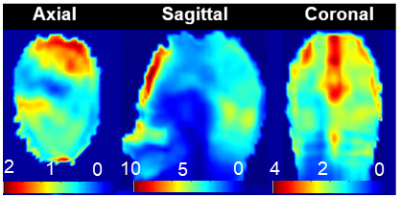
In UHF MRI, higher static field strengths result in higher global specific absorption rate (SAR) values. Additionally, the wave phenomena that emerge in UHF MRI introduce an inherent spatial variation of the electric fields, resulting in a spatially-varying local SAR pattern (Fig. 1). The local variation is hard to predict due to anatomical, tissue compositional and positional variations between patients, as well as variations determined by the transmit RF coil. This increased and difficult to predict local SAR may in fact be the dominant limitation of high field and especially UHF MRI.
Parallel transmit (pTx) technology, in which multiple transmit RF channels can be controlled independently [1],[2], has become popular for mitigating the B1+ field non-uniformity problems that occur at higher field strengths. However, an unconstrained combination of the power output of multiple channels can, in a worst-case scenario, causes very strong local heating effects due to constructive interference of the electric field components from each channel, leading to strong local SAR hotspots, possibly even stronger than those produced by conventional excitation. This concern has led to the development of SAR-aware pTx methods, which employ knowledge of E-fields in addition to the extra degrees of freedom provided by the multi-transmit coil, to reduce local SAR hotspots while simultaneously constraining B1+ inhomogeneity [3]-[8].
Electromagnetic Simulations as the basis for safe and efficient MRI exams
To date there is still no good method available to directly and non-invasively measure local SAR in-vivo. In the current practical environment the global or average SAR is measured and a conservative estimate of the peak local SAR is established using a ratio that is typically in the range between 3:1 and 20:1 [9]. The peak local SAR can then be estimated from the measured global SAR by multiplication with this ratio.
Electromagnetic modeling has become a popular tool to assess SAR in simulation [10]-[14]. A diverse family of detailed body models can be used to estimate global SAR and peak local SAR in various different body types ranging from infants to adults of different gender. While SAR values can still vary from patient to patient, with patient position, and with other variables, these simulations provide a strong basis for novel approaches that tackle SAR prediction more accurately [15]-[17]. Given the strong incentive to develop UHF MRI into a clinical tool, it is paramount to find a viable and accurate method for monitoring the spatially varying SAR pattern, and therefore the actual ratio of peak local SAR to global SAR, as the key parameter in MRI safety. This talk will focus on the simulation methods available today for use in MRI RF heating safety assessment.
Acknowledgements
No acknowledgement found.References
[1] Zhu Y. 2004. Parallel excitation with an array of transmit coils. Magn Reson Med 51(4):775-84.
[2] Katscher U, Börnert P, Leussler C, van den Brink JS. 2003. Transmit SENSE. Magn Reson Med 49(1):144-50.
[3] Martin A, Schiavi E, Eryaman Y, Herraiz JL, Gagoski B, Adalsteinsson E, Wald LL, Guerin B. 2016. Parallel transmission pulse design with explicit control for the specific absorption rate in the presence of radiofrequency errors. Magn Reson Med 75(6):2493-504.
[4] Graesslin I, Vernickel P, Börnert P, Nehrke K, Mens G, Harvey P, Katscher U. 2015. Comprehensive RF safety concept for parallel transmission MR. Magn Reson Med 74(2):589-98.
[5] Guérin B, Setsompop K, Ye H, Poser BA, Stenger AV, Wald LL. 2015. Design of parallel transmission pulses for simultaneous multislice with explicit control for peak power and local specific absorption rate. Magn Reson Med 73(5):1946-53.
[6] Guérin B, Gebhardt M, Cauley S, Adalsteinsson E, Wald LL. 2014. Local specific absorption rate (SAR), global SAR, transmitter power, and excitation accuracy trade-offs in low flip-angle parallel transmit pulse design. Magn Reson Med 71(4):1446-57.
[7] Pendse M, Rutt BK. 2015. IMPULSE: A Generalized and Scalable Algorithm for Joint Design of Minimum SAR Parallel Transmit RF Pulses. Proc Int Soc Magn Res 23:0543.
[8] Seifert F, Wübbeler G, Junge S, Ittermann B, Rinneberg H. 2007. Patient safety concept for multichannel transmit coils. J Magn Reson Imaging 26(5):1315-21.
[9] IEC 60601-2-33
[10] Vaughan JT, Snyder CJ, DelaBarre LJ, Bolan PJ, Tian J, Bolinger L, Adriany G, Andersen P, Strupp J, Ugurbil K. 2009. Whole-body imaging at 7T: preliminary results. Magn Reson Med (1):244-8.
[11] Hand JW, Lau RW, Lagendijk JJ, Ling J, Burl M, Young IR. 1999. Electromagnetic and thermal modeling of SAR and temperature fields in tissue due to an RF decoupling coil. Magn Reson Med 42(1):183-92.
[12] Gandhi OP, Chen XB. 1999. Specific absorption rates and induced current densities for an anatomy-based model of the human for exposure to time-varying magnetic fields of MRI. Magn Reson Med 41(4):816-23.
[13] Simunić D, Wach P, Renhart W, Stollberger R. 1996. Spatial distribution of high-frequency electromagnetic energy in human head during MRI: numerical results and measurements. IEEE Trans Biomed Eng 43(1):88-94.
[14] Neufeld E, Fuetterer M, Murbach M, Kuster N. 2015. Rapid method for thermal dose-based safety supervision during MR scans. Bioelectromagnetics 36(5):398-407.
[15] Pendse M, Stara R, Mehdi Khalighi M, Rutt B. IMPULSE : A scalable algorithm for design of minimum specific absorption rate parallel transmit RF pulses. Magn Reson Med. 2019 Apr;81(4):2808-2822.
[16] Winkler SA, Picot PA, Thornton MM, Rutt BK. Direct SAR mapping by thermoacoustic imaging: A feasibility study. Magn Reson Med. 2017 Oct;78(4):1599-1606.
[17] Dixit N, Stang PP, Pauly JM, Scott GC. Thermo-Acoustic Ultrasound for Detection of RF-Induced Device Lead Heating in MRI. IEEE Trans Med Imaging. 2018 Feb;37(2):536-546.