Use of Intraoperative MRI for Improvement of Neurosurgical Intervention
Akira Matsumura1, Hiroyoshi Akutsu1, Yosuke Masuda1, Tomohiko Masumoto2, Masahide Matsuda1, and Eiichi Ishikawa1
1Department of Neurosurgery, University of Tsukuba, Tsukuba Science City, Japan, 2Department of Radiology, University of Tsukuba, Tsukuba Science City, Japan
Synopsis
Intraoperative MRI (i-MRI) is a powerful tool in improving the surgical intervention for brain and skull base surgery. We would like to share our experience of tha advantage of using i-MRI for better treatmet results.
Use of Intraoperative MRI for Improvement of Neurosurgical Intervention
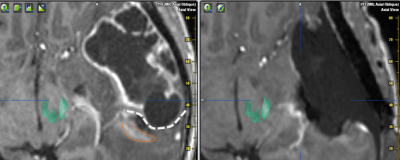
In this lecture, review of various type of intraoperative MRI will be introduced and its benefit and limitation will be discussed. Additionally, the authors own experience using high-filed intraoperative MRI (i-MRI) for glioma surgery and skull base surgery will be presented. From 2015 to 2018, i-MRI has been applied in 389 cases. There were 270 cases with open craniotomy, 86 cases for trans-sphenoidal surgery and 33 cases for biopsy and the mean age was 51.4+20.6 years old. For glioma surgery, Gross total removal rate was 89.6% in non-eloquent area and preservation for the motor function was 94% and was 92% for language function in near eloquent area tumors (< 1cm). For trans-sphenoidal surgery, there was 50 pituitary adenoma (PA), followed by Chordoma, Craniopharyngioma, skull base meningioma. In PA, gross total removal rate was 55%. This seems to be not so high, however the purpose of using MRI is to identify the important anatomy such as carotid artery, cavernous sinus, cranial nerves (especially optic nerve and performing safe tumor removal according the i-MRI. For tissue biopsy surgery , there were sampling error before i-MRI in 25.9% of the cases and after confirming the location of the tumor using i-MRI the success rate was 100%. Conclusion Usage of i-MRI improve the extent of the tumor removal in glioma and other intracranial tumors by detecting the unexpected tumor residual. For trans-sphenoidal or trans-oral surgery, it is useful to identify important anatomy to prevent unwanted complication for the excessive surgery.For biopsy of the tissue sample, i-MRI improve the sampling error rate after first trial and it is especially useful in small lesions.