4095
Free-Breathing Dynamic Contrast-Enhanced Magnetic Resonance Imaging of the Lung Using Compressed-Sensing VIBE1Department of Radiology, Hua Dong Hospital,Fudan University, Shanghai, China, 2MR Application Development, Siemens Shenzhen Magnetic Resonance Ltd, Shenzhen, China, 33. MR Application Predevelopment, Siemens Healthcare, Erlangen, Germany
Synopsis
The purpose of this study was to compare the image quality of free-breathing
CS-VIBE and TWIST-VIBE in patients with lung disease. In patients who were able
to hold their breath well, the images quality of CS-VIBE and TWIST-VIBE were
comparable (P>0.05). In patients who
failed to hold their breath during the required period, CS-VIBE allowed for
superior image quality, lesion delineation, artifact level, and diagnostic
confidence compared to TWIST-VIBE. Our study demonstrated that free-breathing
CS-VIBE is feasible for lung imaging for patients who have difficulties holding
their breath.
Introduction
Several studies[1][2] have demonstrated that dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) is a promising technique for assessing lung pathology. Unfortunately, conventional DCE-MRI of the lung often suffers from respiratory motion artifact due to the long scan time required by DCE-MRI. Although k-space data sharing techniques, such as TWIST, could improve the temporal resolution of DCE-MRI, it is still sensitive to motion artifact and requires breath-holding. However, various studies have reported promising results using the compressed sensing (CS) technique, which can significantly accelerate MRI acquisition time by acquiring less k-space data. In the present study, we assess the feasibility of free-breathing dynamic lung imaging using CS-VIBE.
Methods
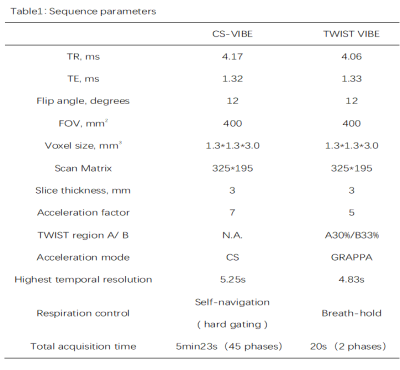
30 patients (16 male, 14 female), with lung lesions detected on
computed tomography (CT), underwent free-breathing dynamic enhancement imaging
using a prototype CS-VIBE sequence (45 phases, 5min 21s) immediately followed
by a TWIST VIBE sequence (breath-hold, 2 phases with 20s) in the delayed phase for
comparison purposes. All MRI examinations were performed on a 3T scanner
(MAGNETON Prisma, Siemens Healthcare, Erlangen, Germany). The parameters of
both sequences are shown in Table 1. For CS-VIBE sequence, a motion-dominated navigation
signal was acquired along with the image data, and the hard-gating
mode based on the navigation signal was used to eliminate the respiratory
motion artifact [3]. Patients were divided by the technician into a cooperative
group (n=12) and a non-cooperative group (n=18) according to their ability to
successfully hold their breath. Two experienced radiologists blindly scored
overall image quality, lesion delineation, overall artifact level, and
diagnostic confidence of the CS-VIBE (the latest phase ) and the TWIST VIBE (
the first phase ) images for each case using a Likert-type scale (for the image
quality, 4 = good, 3 = adequate, 2 = borderline, and 1 = nondiagnostic; for the
delineation of lesions, 4 = sharp margins, 3 = slight blurring, 2 = moderate
blurring, and 1 = nondiagnostic; for the overall
artifact level, 4 = no artifact, 3 = mild artifact, 2 = significant artifact, 1
= nondiagnostic; for the diagnostic confidence, 3 = good confidence, 2 = moderate
confidence, and 1 = nondiagnostic)[4]. Intraclass correlation coefficients (ICCs) were calculated for
inter- and intra-observer variability.Results
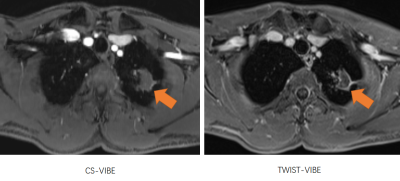
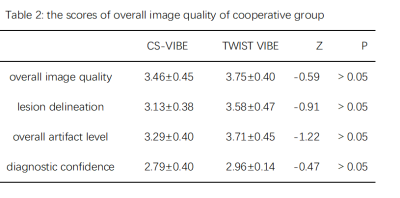
The image quality of the free-breathing CS-VIBE and TWIST-VIBE
sequences were comparable within the cooperative group (P>0.05)(Table2). Figure 1 shows a typical case from the cooperative
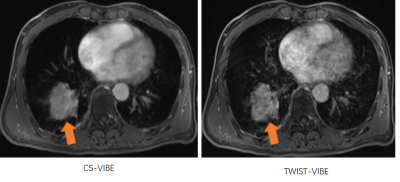
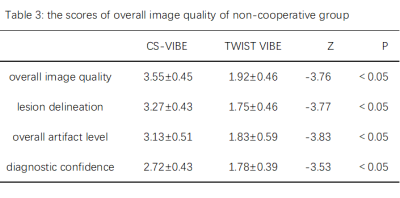
group. Within the non-cooperative group, the scores of the overall image quality, lesion
delineation, overall artifact level, and diagnostic confidence for CS VIBE were significantly higher than TWIST-VIBE (P<0.05)(Table3) . Figure 2 demonstrates a
representative case from the non-cooperative group. The image quality of
CS-VIBE was not significantly different between the cooperative group and
non-cooperative group. ICCs for intra- and inter-observer variability were 0.696–0.900
and 0.702–0.901, respectively.Discussion
By incoherently acquiring a subset of the
k-space data and constraining the reconstruction to support certain sparsity
properties, compressed sensing can accelerate MRI scan time and achieve
artifact-free images [1]. Vreemann
S et al.[5] found that CS-VIBE could obtain higher spatial
resolution for breast DCE-MRI than TWIST-VIBE with a similar temporal
resolution while the image quality of both was comparable. Moreover, CS-VIBE was
less susceptible to movement artifact compared to TWIST-VIBE. In a study on
liver DCE-MRI[3],
a similar CS-VIBE sequence with what we used in our study was found to be
immune to motion artifact in patients with limited breath-holding capacity or transient
dyspnea after gadoxetic acid administration, allowing for consecutive
multi-phase dynamic contrast-enhanced imaging during
free breathing. In our study, we applied the free-breathing CS-VIBE to the consecutive
multi-phase DCE for the lung. Our findings agreed with these previous studies
above. For patients who have limited breath-holding capacity, free-breathing
CS-VIBE could achieve artifact-free images, which indicates that CS-VIBE could
be the potentially preferred alternative for lung DCE-MRI when patients are at
high risk of having difficulty holding their breaths.Conclusion
Acknowledgements
No acknowledgement found.References
[1] Yuan M, Zhang Y D, Zhu C, et al. Comparison of intravoxel incoherent motion diffusion-weighted MR imaging with dynamic contrast-enhanced MRI for differentiating lung cancer from benign solitary pulmonary lesions[J]. J Magn Reson Imaging, 2016,43(3):669-679.
[2] Wang L L, Lin J, Liu K, et al. Intravoxel incoherent motion diffusion-weighted MR imaging in differentiation of lung cancer from obstructive lung consolidation: comparison and correlation with pharmacokinetic analysis from dynamic contrast-enhanced MR imaging[J]. Eur Radiol, 2014,24(8):1914-1922.
[3] Yoon J H, Yu M H, Chang W, et al. Clinical Feasibility of Free-Breathing Dynamic T1-Weighted Imaging With Gadoxetic Acid-Enhanced Liver Magnetic Resonance Imaging Using a Combination of Variable Density Sampling and Compressed Sensing[J]. Invest Radiol, 2017,52(10):596-604.
[4] Chen L, Liu D, Zhang J, et al. Free-breathing dynamic contrast-enhanced MRI for assessment of pulmonary lesions using golden-angle radial sparse parallel imaging[J]. J Magn Reson Imaging, 2018. [5] Vreemann S, Rodriguez-Ruiz A, Nickel D, et al. Compressed Sensing for Breast MRI: Resolving the Trade-Off Between Spatial and Temporal Resolution[J]. Invest Radiol, 2017,52(10):574-582.
Figures