3167
Decreased FDG-PET Uptake and Inter-Hemispheric Functional and Structural Connectivity in Patients with Multi-domain Amnestic Mild Cognitive Impairment1The 2nd Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou, China, 2GE Healthcare Shanghai, Shanghai, China
Synopsis
Amnestic mild cognitive impairment (aMCI) is not a uniform disease entity. Based on clinical symptoms, aMCI can be further classified as single-domain aMCI (SD-aMCI) with isolated memory deficit, or multi-domain aMCI (MD-aMCI) if memory deficit is combined with other cognitive domains impairment. By examining cerebral metabolism, inter-hemispheric connectivity, behavioral features, and neuropathologies, we observed disrupted bilateral cerebral metabolism, structural and functional disconnection between bilateral hemispheres in MD-aMCI, but not in SD-aMCI. Thus, along with the continuum between normal aging and Alzheimer’s disease, SD-aMCI and MD-aMCI may represent two clinical phases.
Synopsis
Amnestic mild cognitive impairment (aMCI) is not a uniform disease entity. Based on clinical symptoms, aMCI can be further classified as single-domain aMCI (SD-aMCI) with isolated memory deficit, or multi-domain aMCI (MD-aMCI) if memory deficit is combined with other cognitive domains impairment. By examining cerebral metabolism, inter-hemispheric connectivity, behavioral features, and neuropathologies, we observed disrupted bilateral cerebral metabolism, structural and functional disconnection between bilateral hemispheres in MD-aMCI, but not in SD-aMCI. Thus, along with the continuum between normal aging and Alzheimer’s disease, SD-aMCI and MD-aMCI may represent two clinical phases.Introduction
According to the clinical symptom, aMCI patients can be further divided into two subtypes: SD-aMCI, characterized by selective episodic memory impairment, and MD-aMCI, presenting widespread deficits in at least one other cognitive domain, including processing speed, executive function, or visuospatial abilities1. MD-aMCI have a greater risk of clinical progression than SD-aMCI.
Robust inter-hemispheric connectivity is one of the modes of the brain’s intrinsic functional architecture, which has rarely been investigated in patients with different aMCI subtypes. Prior work showed AD patients had the deficit in the inter-hemispheric integration of information. Specifically, AD patients can normally perform in tasks relied on intra-hemispheric processing while performed poorly when inter-hemispheric communication was required. Thus, by examining cerebral metabolism, inter-hemispheric connectivity, behavioral features, and neuropathological biomarkers, our study aims to explore the divergent neural mechanism underlying aMCI subtypes.
Methods
All subjects underwent a battery of neuropsychological tests to assess general mental status and other cognitive domain, including memory function. Impairment was defined by the presence of a test scoring 1.5 standard deviations below the average score of age and education-matched healthy controls. Therefore, we divided 64 aMCI patients into 32 SD-aMCI and 32 MD-aMCI subsequently (Table 1). Moreover, our study sought to examine the PET-FDG uptake value, inter-hemispheric resting-state functional and structural connectivity. Specifically, we focused particularly on cerebral metabolisms in bilateral predefined regions (including posterior cingulate cortex, bilateral inferior temporal gyrus, and angular gyrus), voxel-mirrored homotopic connectivity and volume of corpus callosum subregions. Also, we achieved the CSF sample from subjects.Results
Findings that regions show decreased inter-hemispheric functional connectivity overlap well with bilateral glucose hypometabolism. MD-aMCI patients showed decreased PET-FDG uptake in all predefined regions, and the bilateral decreased inter-hemispheric functional connectivity in the precuneus (PCu), middle temporal gyrus, calcarine gyrus (CG), and postcentral gyrus. Moreover, atrophy of mid-posterior corpus callosum was also found in MD-aMCI. By comparison, no significant differences of indices were found between SD-aMCI patients and controls (Figure 1, 2, Table 2). Besides, decreased PET-FDG uptake in inferior temporal gyrus and angular gyrus was related to increased level of p-tau181 within aMCI patients (Figure 3).Discussion
To the best of our knowledge, this is the first research to investigate cerebral metabolism and inter-hemispheric functional and structural connectivity in patients with different aMCI subtypes. The present study yielded evidence that MD-aMCI had simultaneously decreased cerebral metabolism and reduced inter-hemispheric homotopic RSFC in similar brain regions, and corresponding atrophy of mid-posterior CC when compared to SD-aMCI and NC.
Specifically, MD-aMCI displayed decreased glucose metabolism in bilateral ITG and reduced RSFC between bilateral MTG relative to SD-aMCI and NC. These brain regions we identified were mainly located within the memory-related network. The PCu has reciprocal cortico-cortical connections with the PCC. Our results indicated MD-aMCI had reduced inter-hemispheric RSFC and metabolism in PCC/PCu. Moreover, the RSFC between bilateral PCu was associated with executive function. Concerning the lateral parietal lobe, MD-aMCI group exhibited hypometabolism in bilateral AG and reduced bi-hemispheric PCG RSFC relative to SD-aMCI and NC. Besides, MD-aMCI patients had significantly reduced inter-hemispheric RSFC in bilateral CG, which are part of the extra-striate visual network and involve with the perception created by visual stimuli. As the central white matter pathways, the CC links cortical hubs of the left and right hemispheres together. Our results showed MD-aMCI group had decreased mid-posterior CC volume as compared to SD-aMCI and NC, corrected by total intracranial volume.
However, no such differences were found between SD-aMCI and NC. Correlation analyses showed different neuroimaging indices were associated with behavioral data, including general cognitive abilities and executive function, suggesting their potential clinical value as biomarkers to estimate the risk of the AD. Notably, only the index of metabolism showed a tight correlation with misfolded tau protein. Together, our findings demonstrate that patients with MD-aMCI have more compound neuropathological mechanism relative to SD-aMCI.
Conclusion
MD-aMCI group had severe impairment of inter-hemispheric cooperation while SD-aMCI group relatively preserved it. Furthermore, we explored the possible mechanism underlying the deficits in inter-hemispheric connectivity and hypothesized that abnormal accumulation of misfolded tau proteins might be the initial factor to trigger a series of downstream events.Acknowledgements
No acknowledgement found.References
1Winblad, B., Palmer, K., Kivipelto, M., Jelic, V., Fratiglioni, L., Wahlund, L.O., et al. (2004). Mild cognitive impairment – beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. Journal of Internal Medicine 256(3), 240-246.Figures

Table 1
Abbreviation: MMSE: Mini-Mental State Examination; ADAS, the Alzheimer's Disease Assessment Scale-cognitive subscale; WMS-LM, Wechsler memory scale-logical memory; TMT, Trail-Making Test; CSF: cerebrospinal fluid;CDT,clock drawing test;AVLT, auditory verbal learning test;BNT, Boston naming test.
a post-hoc paired comparisons showed significant group differences between NC and SD-aMCI, after Bonferroni correction (p<0.05). b post-hoc paired comparisons showed significant group differences between NC and MD-aMCI, after Bonferroni correction (p<0.05). c post-hoc paired comparisons showed significant group differences between SD-aMCI and MD-aMCI, after Bonferroni correction (p<0.05).
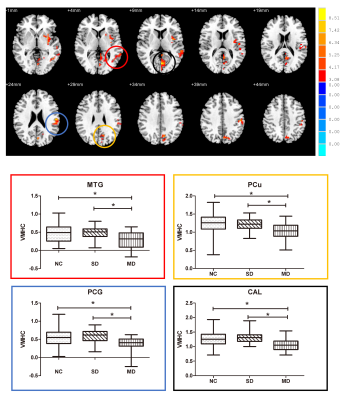
Figure 1
Upper: Brain areas with the significant difference of VMHC among normal controls, SD-
Lower: post-hoc analyses were performed within the areas identified by the ANOVA (corrected by Bonferroni, p<0.005). MD-
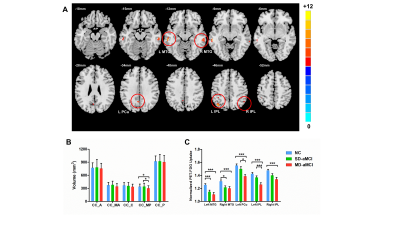
Figure 2
A. Histograms of FDG-ROIs are shown for MD-aMCI, SD-aMCI, and normal controls. Error bars represent standard deviation. We found that MD-aMCI patients had significantly decreased PET-FDG uptake value compared to the other two groups (p<0.005, corrected). B. The volume of corpus callosum sub-regions in three groups. MD-aMCI showed the significantly decreased volume of CC-MP compared to other two groups (p<0.05, corrected); Abbreviation: A: anterior; MA: mid-anterior; C: central; MP: mid-posterior; P: posterior.
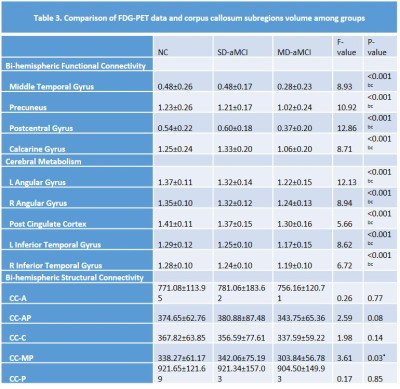
Table 2
Data are presented as means ± standard deviations. Abbreviation: CC: corpus callosum; A: anterior; MA: mid-anterior; C: central; MP: mid-posterior; P: posterior
a post-hoc paired comparisons showed significant group differences between NC and SD-aMCI, after Bonferroni correction (p<0.05).
b post-hoc paired comparisons showed significant group differences between NC and MD-aMCI, after Bonferroni correction (p<0.05).
c post-hoc paired comparisons showed significant group differences between SD-aMCI and MD-aMCI, after Bonferroni correction (p<0.05).
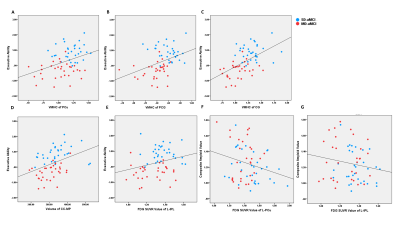
Figure 3
Scatter plot: the blue and red dot represents the SD-aMCI and MD-aMCI patients respectively. A: PET-FDG uptake value in right AG was related to log-transformed ADAS-cog (r=-0.39, p<0.001); B: PET-FDG uptake value in right AG was related to level of p-tau181 (r=-0.42, p<0.001); C: PET-FDG uptake value in left ITG was related to p-tau181 (r=-0.44, p<0.001); D-F: regarding functional connectivity, reduced inter-hemispheric functional connectivity in PCu (r=0.39, p<0.001), PCG (r=0.40, p<0.001) and CG (r=0.54, p<0.001) were related to composite score of executive function; G: the CC-MP volume was related to composite score of executive function (r=0.40, p<0.001).