2968
Inefficient cranial venous outflow in patients with Meniere’s disease1Radiology, Santa Maria del Carmine, Rovereto, Italy, 2Center for Mind/Brain Sciences, University of Trento, Rovereto, Italy, 3Computational Life Inc., Delaware, DE, United States, 4Otorhinolaryngology, Dr, Rovereto, Italy, 5DICAM, Laboratory of Applied Mathematics, University of Trento, Trento, Italy
Synopsis
Meniere’s disease (MD) patients have a high incidence of abnormal neck venous vessels. This results in hampered cerebral venous outflow, disturbed intracranial dynamics, hampered CFS reabsorption, increased venous pressure and intracranial pressure (ICP), disturbed inner ear circulation and possibly disturbed perilymphatic and endolymphatics fluid spaces. Such disturbed intracranial dynamics may help explain endolymphatic hydrops and underlying mechanisms in MD. In this study we performed magnetic resonance venography (MRV) and phase contrast MRI (PC-MRI) in patients with MD to study the anatomy of the extracranial venous vessels and flow in various cranial compartments.
ABSTRACT
Meniere’s disease (MD) patients have a high incidence of abnormal neck venous vessels. This results in hampered cerebral venous outflow, disturbed intracranial dynamics, hampered CFS reabsorption, increased venous pressure and intracranial pressure (ICP), disturbed inner ear circulation and possibly disturbed perilymphatic and endolymphatics fluid spaces. Such disturbed intracranial dynamics may help explain endolymphatic hydrops and underlying mechanisms in MD. In this study we performed magnetic resonance venography (MRV) and phase contrast MRI (PC-MRI) in patients with MD to study the anatomy of the extracranial venous vessels and flow in various cranial compartments.INTRODUCTION
MD is a multifactorial disease clinically characterized by intermittent severe bouts of vertigo, tinnitus and aural pain. There is evidence to suggest that altered venous drainage of the inner ear may be frequent in patients with Ménière’s disease (MD) 1,2. This would result in altered fluid circulation in the inner ear and can cause a permanent increase in the volume of the endolymph, a condition also termed endolymphatic hydrops (EH). Since the endolymphatic space in the inner ear communicates directly with the subarachnoid space, an increase in intracranial pressure will be transmitted to the inner ear and cause MD. Recent literature points to the presence of extracranial venous anomalies in 83% of the patients, potentially leading to reduced venous outflow and increased intracranial pressure 3. To this effect, venous angioplasty may be a potential treatment 4.MATERIALS AND METHODS
T1 structural MRI data was used to characterize segment the three tissue types in the brain: CSF, white matter (WM) and gray matter (GM) in 16 patients with MD and matched to similar data already available in literature. Phase contrast magnetic resonance imaging (PC-MR) was performed at the level of the aqueduct of Sylvius (AoS) and the cervical spine C2C3 level to quantify CSF flow and calculate total arterial input and venous output in and out of the intracranial cavity (Figure 1). Contrast-enhanced magnetic resonance venography (MRV) was performed to characterize any venous anomalies in the dural sinuses and the extracranial neck vessels. All data was collected on a 1.5T Siemens clinical scanner in a local hospital.RESULTS (work in progress)
total intracranial volume of 1417.45cc was within normal values (1367.3±147.4cc), however there was increased total CSF volume 308,16cc (normal 151±54cc) and reduced GM volume 567,06cc (normal 717±96.8), whereas WM volume was found to be within normal range of 558.66cc (499.9±73.7cc). Flow data could be calculated on 12 patients (4 were excluded due to the presence of artifacts). All patients presented with varying degrees of IJV stenosis and anomalous venous drainage pattern that included recruitment and enlargement of additional draining veins in the neck (Figure 2). Total IJV/totalA was was 61.6±25.8 with respect to normal 71.1±22 5.DISCUSSION
All our patients demonstrated anomalous venous anatomy and increase number of tortuous veins in the neck (Figure 2). tIJV/tA had a trend to be lower with respect to healthy controls suggesting that patients with MD are more likely to have an inefficient venous outflow with respect to healthy controls. This would lead to increase in intracranial venous volume and pressure, altering CSF reabsorption via the subarachnoid granulation further increasing intracranial pressure. Our segmentation results suggest a very high total CSF volume in patients, a reduced total GM volume whereas total WM remained within the normal change. The theoretical study of Toro et al. (2018) confirms the expectation of increased CSF pressure, increased inner ear venous pressure and disrupted inner ear circulation. This is crucial to begin to understand the underlying mechanisms of MD, as CSF is directly connected to the perilymphatic space through the cochlear aqueduct. Increased CSF pressure may disturb the dynamics of perilymphatic and endolymphatic fluids and possibly explain rupture of their separating membrane, the endolabyrinthine membrane (the Reissner membrane). Membrane rupture would cause potassium intoxication of the perilymphatic fluid and disturb neurotransmission, recalling that perilymphatic fluid has electrolyte levels similar to CSF, suitable for neural transmission. More experimental and clinical work is required to confirm (or deny) these results and to begin constructing a biophysical framework to understand MD and to propose appropriate therapies.Acknowledgements
No acknowledgement found.References
1. Gussen R. Vascular mechanisms in Meniere's disease. Otolaryngol Head Neck Surg. 1983;91:68–71. 2. Friis M, Qvortrup K. A Potential Portal Flow in the Inner Ear. The Laryngoscope. 2007;117:194–198. 3. Di Berardino F, Alpini DC, Bavera PM, et al. Chronic cerebrospinal venous insufficiency in Ménière disease. Phlebology. 2nd ed. 2014;30:274–279.
4. Bruno A, Napolitano M, Califano L, et al. The Prevalence of Chronic Cerebrospinal Venous Insufficiency in Meniere Disease_ 24-Month Follow-up after Angioplasty. JVIR. Elsevier Inc; 2017;28:388–391.
5. Lagana MM, Chaudhary A, Balagurunathan D, et al. Cerebrospinal fluid flow dynamics in multiple sclerosis patients through phase contrast magnetic resonance imaging. 2014;11:349–358.
6. Toro EF, Borgioli F, Zhang Q, Contarino C, Müller LO, Bruno A. Inner-ear circulation in humans is disrupted by extracranial venous outflow strictures: Implications for Ménière’s disease. Veins and Lymphatics. 2018;7:1–12.
Figures
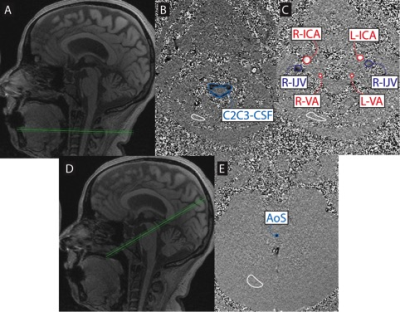



Figure 4: 51yr old female. MRV images show tortuous and dilated right deep cervical vein.