2955
The differentiation between sinonasal natural killer/T-cell lymphomas and diffuse large B-cell lymphomas by high resolution DWI combined with conventional MRIMengge He1, Zuohua Tang1, zebin xiao1, Linying Guo1, and Zhongshuai Zhang2
1EENT Hospital of Fudan University, Shanghai, China, 2SIEMENS Healthcare, Diagnostic Imaging, Shanghai, China
Synopsis
Previous studies already reported that RESOLVE DWI can
significantly reduce the susceptibility induced image distortion artifacts [1;
2; 3]. This study used RESOLVE DWI and
conventional MRI to differentiate sinonasal natural killer/T-cell lymphomas
from diffuse large B-cell lymphomas.
Purpose
To explore the feasibility of discrimination between natural killer (NK)/T-cell lymphomas (NKTLs) and diffuse large B-cell lymphomas (DLBCLs) using the readout segmented EPI (RESOLVE) diffusion-weighted imaging (DWI) technique combined with conventional magnetic resonance imaging (MRI).Materials and Methods:
Sixty-five patients (46 females, 19 males; mean age, 59.6 ± 14.1 years) with sinonasal lymphomas underwent RESOLVE DWI as well as conventional MRI (T1W, T2W and contrast-enhanced T1WI with fat suppression). All the exams were performed on a 3T MR scanner (MAGNETOM Verio, Siemens Healthcare, Erlangen, Germany). The enrolled 65 patients include 45 NKTLs (35 men and 10 women; mean age, 57.5 ± 15.1 years) and 20 DLBCLs (11 men and 9 women; mean age, 60.9 ± 11.7 years) and both groups were confirmed by histopathology. Apparent diffusion coefficient (ADC) value acquired by RESOLVE and conventional MRI features were compared between NKTLs and DLBCLs using multivariate logistic regression. Receiver operating characteristic (ROC) curve analysis was performed to determine the optimal cut-off ADC value and diagnostic performance in distinguishing between NKTLs and DLBCLs. The area under the curves (AUCs) were compared between conventional MRI and a combination with DWI.Results:
As shown in Fig 1, for differentiating between NKTLs and DLBCLs, by using conventional MRI (tumor location in nasal cavity for NKTLs versus in paranasal sinus for DLBCLs) the sensitivity, specificity, and AUC were 95.2%, 78.3% and 0.894, respectively.; Those for the combination of conventional MRI and DWI (a cut-off ADC value of 0.646×10-3 mm2/s) 91.7%, 94.0%, and 0.973, respectively. A significant difference of AUC was found between conventional MRI and a combination with DWI (p = 0.02)(Figs 2 and 3). Representative MRI and histopathological images are shown in Figs 4 and 5.Conclusions:
Location was the most valuable conventional MRI feature for differentiating between NKTLs and DLBCLs. A combination of DWI could significantly improve the differential performance.Acknowledgements
This work was supported by the Grant of Science and Technology Commission of Shanghai Municipality (Grant number: 17411962100) and Key Project of the National Natural Science Foundation of China (Grant number: 61731009).References
[1] M. Zhao, Z. Liu, Y. Sha, S. Wang, X. Ye, Y. Pan, and S. Wang, Readout-segmented echo-planar imaging in the evaluation of sinonasal lesions: A comprehensive comparison of image quality in single-shot echo-planar imaging. Magnetic Resonance Imaging 34 (2016) 166-172. [2] F. Wang, Y. Sha, M. Zhao, H. Wan, F. Zhang, Y. Cheng, and W. Tang, High-Resolution Diffusion-Weighted Imaging Improves the Diagnostic Accuracy of Dynamic Contrast-Enhanced Sinonasal Magnetic Resonance Imaging. Journal of Computer Assisted Tomography 41 (2017) 199-205. [3] X. Wang, Z. Zhang, Q. Chen, J. Li, and J. Xian, Effectiveness of 3 T PROPELLER DUO diffusion-weighted MRI in differentiating sinonasal lymphomas and carcinomas. Clinical Radiology 69 (2014) 1149-1156.Figures
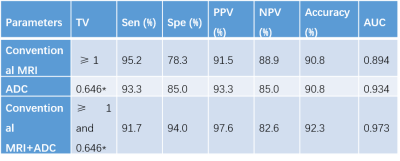
Fig 1. Diagnostic
performance of conventional MRI, ADC value and their combination for
differentiating sinonasal NKTLs from DLBCLs.
TV: threshold value; * × 10-3 mm2/s.
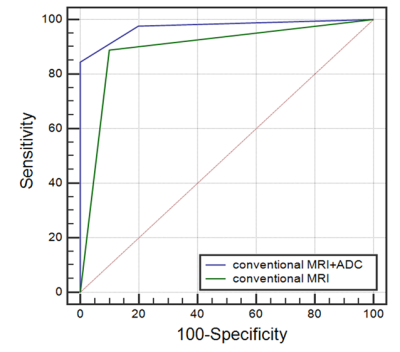
Fig 2 ROC curves of the diagnostic efficacy using conventional MRI, and the combination
of conventional MRI and ADC to differentiate between NKTLs and DLBCLs.
AUC of the combination was significantly
higher than that of conventional MRI (p = 0.02)
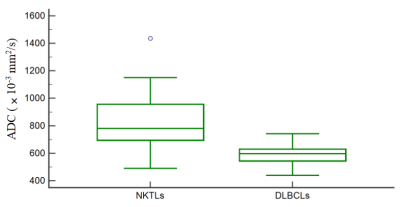
Fig 3 Boxplot shows ADC value (polygonal ROI)
of sinonasal NKTLs and DLBCLs. The mean ADC value is significantly higher in NKTLs than in DLBCLs (p
< 0.001).
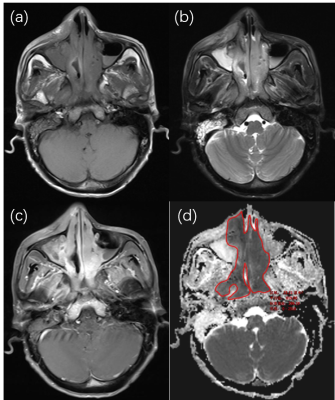
Fig 4. A 56-year-old man
with NKTL in bilateral nasal cavity and nasopharyngeal top. The tumor appears
as an irregular mass with an isointense signal on axial T1-weighted image (a),
a heterogeneously hyperintense signal on T2-weighted image (b) and an intensely
heterogeneous enhancement (c). The tumor invades nasopharyngeal,
pterygopalatine fossa, infratemporal fossa and right upper lip cutaneous
tissues. (d) Axial ADC map (b = 1000 s/mm2) shows the tumor has an
ADC value of 0.819× 10-3 mm2/s using polygonal ROI
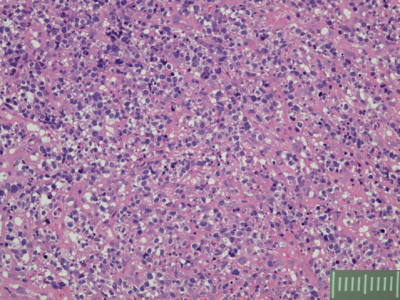
Fig 5. A 42-year-old man with NKTL in
nasal cavity and maxillary
sinus. The neoplasm is composed of a mixture of polymorphous inflammatory cells
(eosinophils, neutrophils, histiocytes
and lymphocytes) and malignant atypical cells,
and is characterized by angiocentricity or angiotropism in which tumor cells
infiltrate and destroy blood vessel walls.