2851
The comparison of L-FBPA PET/MR and PET/CT for BNCT treatment evaluation1Department of Nuclear Medicine, Taipei Veterans General Hosptial, Taipei City, Taiwan, 2Department of Radiation Oncology, Taipei Veterans General Hosptial, Taipei City, Taiwan, 3Biomedical Imaging and Radiological Sciences, National Yang-Ming University, Taipei City, Taiwan
Synopsis
We hypothesized that o-fluoro-L-p-boronophenylalanine (L-18FPBA) PET/MR could provide more
precise treatment planning for Boron neutron capture therapy (BNCT) compared
with L-18FBPA PET/CT. We implemented the phantom trial to measure the radioactivity
correlation between PET/CT and PET/MR. Results have high comparability. We
accessed patients who were potentially eligible for BNCT with same paradigms.
The initial results represented acceptable correlation between these two modalities.
Furthermore, because of high sensitivity and sophisticated imaging resolution,
medics can easy to organize the more accurate treatment planning. In
conclusion, PET/MR provides comparable L-18FBPA quantitative measurement and more
diagnostic accuracy than PET/CT.
Introduction
With the prevalence of BNCT, L-18FPBA became the dominant biomarker for prediction of 10Boron concentration in tumor cells using PET 1-4, especially L-BPA based accumulation in Glioma and melanoma 4-8. However, the concentration accumulations are not only the tumor cells but also in the normal tissue 4, 9. While the recommended radioactivity of L-18FPBA is around 10mCi in theory10, the L-18FPBA productivity can reach at 5mCi in our radiochemistry laboratory. The novel Time-of-flight(TOF) reconstruction in PET/MR can decline the image degradation with 35% of the activity concentration compared with dose concentration in the conventional PET/CT, meanwhile, L-18FBPA-PET remains high image quality and sensitivity 11, 12. Thus, PET/MR could provide images not only with high spatial resolution for region-of-interests (ROIs) recruitment but also feasible quantitative information. Precise ROIs recruitment could decline toxicity of BNCT prediction and improve the treatment efficacy4. To acquire more precise images for the radiotherapy planning and implement assessments within optimal scanning time, the PET/MR could be the pioneer means for L-18FBPA evaluation.Methods
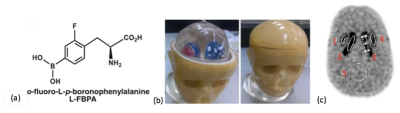
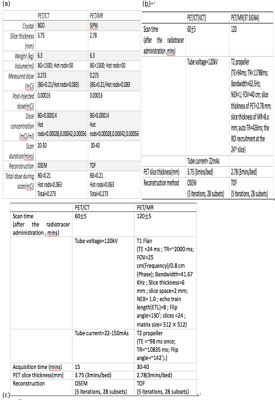
In the phantom trial, the Striatum phantom (RS-901T; Radiology Support Devices Inc.) with weight=6.3 kg, total density=1.1 g/ml, mass density of cortical bone= 1.86 g/ml and 5 subsegmentations as Figure 1-b&c, was conducted to prove feasibility of the hypothesis. Because the fructose is sustainablely labeled on the BPA and a monosaccharide as same as glucose, therefore,phantom was prepared following by table 1 with L-18F-FDG 0.273mCi. The phantom parameters were implemented by PET/CT (VCT, GE Healthcare,USA) and PET/MR (3T SIGNA, GE Healthcare,USA). The PET/CT and PET/MR paradigms were demonstrated as Figure 2 a-b. All patients was divided into 3 groups by pathological diagnoses as Glioblastoma & Anaplastic Astrocytoma (GBM&AA), Head&Neck (H&N) and Others. The L-18FBPA injection administration was 5.858±0.918 mCi. The parameters of PET/CT and PET/MR were shown as Figure 2 c. The reconstruction methods were implemented by Ordered subset expectation maximization (OSEM) in PET/CT and time-of-flight (TOF) in PET/MR respectively. All ROIs recruitment follows with the activity threshold 50% as Figure 1 c. The algorithm of standardized uptake value ratio (SUVR), tumor-to-normal ratio (T/N), as equal [1].SUVR=SUV tumour/SUV normal [1]
Where, the normal is muscle with 1.0±0.1 g/ml within 10x10 mm2.
Results
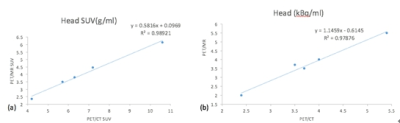
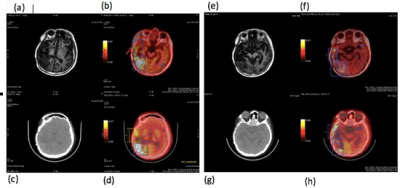
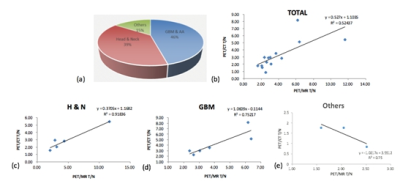
In the phantom trial, Mean SUV (g/ml) results were 4.2 to 10.6 using PET/CT and 2.36 to 6.15 using PET/MR respectively. Mean radioactivity (kBq/ml) were 3.5 to 5.4 by PET/CT and 2 to 5.5 by PET/MR respectively. In the patient trials, the mean scanning times were 20~25 mins in PET/CT and 30~40 mins in PET/MR respectively. The interval time between PET/CT and PET/MR was 60±25mins. SUVRs depending on the mass size and cellular component are 4.933±4.499 in PET/CT and 2.989±1.741 in PET/MR for the H&N group, 3.385±1.629 and 3.399±1.966 for the GBM&AA group, 2.05±0.46 and 1.456±0.543 for the other cancers respectively. Figure 4 represented the one of GBM patient’s 18FBPA PET/CT and PET/MR results.Discussion
Due to the highly correlation in the phantom trial, the hypothesis of the feasibility of L-18FBPA-BNCT in PET/MR is practical. The Pearson correlation of SUVRs and radioactivity between PET/CT and PET/MR were 0.989 and 0.978 as Figure 3. The overall T/N comparison of PET/CT and PET/MR was 0.524. In the GBM&AA and other cancer group, the T/Ns were around 0.752 as Figure 5. In the H&N group, the T/N reached at 0.918. Because the acquisitions were implemented by TOF technique, the spatial resolution is superior to the conventional OSEM method, especially for the ROIs recruitment of minor lesions. PET/MR can demonstrate the minor lesions and recurrence by different sequences. By far, the T/N ratio was determined by operator’s experience; therefore, the high resolution approach can improve the accuracy of ROIs recruitment. Another problem of PET/CT and PET/MR was installed in the different venues at our department temporarily. Although optimal scanning time was traded off and the magnitudes of L-18FBPA declined sharply as Figure 5 e, the outcomes coming from PET/MR reached credits to measure acceptable SUVRs for BNCT evaluations.Conclusion
Even if the integrated PET/MR can provide superior image acquisition to BNCT ROIs assessments, the radioactivity was trade-off because of the delayed scan timing and more complex metabolism in each tumor cells, especially GBM. By our initial experience, the H&N assessments were highly recommended by L-18FBPA-PET/MR due to the highly correlation outcomes. To clarify metabolic surveillance in specific tumor cells, the dose distribution of 18FBPA should be evaluated by specific MR sequences and can be the future direction to improve accuracy of planning. In short, PET/MR could become an alternative and feasible approach to evaluate L-18FBPA-PET instead of traditional L-18FBPA-PET/CT.Acknowledgements
No acknowledgement found.References
1. Ishiwata K, Ido T, Mejia AA, Ichihashi M, Mishima Y. Synthesis and radiation dosimetry of 4-borono-2-[18F]fluoro-D,L-phenylalanine: a target compound for PET and boron neutron capture therapy. Int J Rad Appl Instrum A. 1991;42(4):325-8.
2. Henriksson R, Capala J, Michanek A, Lindahl SA, Salford LG, Franzen L, et al. Boron neutron capture therapy (BNCT) for glioblastoma multiforme: a phase II study evaluating a prolonged high-dose of boronophenylalanine (BPA). Radiother Oncol. 2008;88(2):183-91.
3. Wang HE, Liao AH, Deng WP, Chang PF, Chen JC, Chen FD, et al. Evaluation of 4-borono-2-18F-fluoro-L-phenylalanine-fructose as a probe for boron neutron capture therapy in a glioma-bearing rat model. J Nucl Med. 2004;45(2):302-8.
4. Wingelhofer B, Kreis K, Mairinger S, Muchitsch V, Stanek J, Wanek T, et al. Preloading with L-BPA, L-tyrosine and L-DOPA enhances the uptake of [(18)F]FBPA in human and mouse tumour cell lines. Appl Radiat Isot. 2016;118:67-72.
5. Capuani S, Gili T, Bozzali M, Russo S, Porcari P, Cametti C, et al. L-DOPA preloading increases the uptake of borophenylalanine in C6 glioma rat model: a new strategy to improve BNCT efficacy. Int J Radiat Oncol Biol Phys. 2008;72(2):562-7.
6. Capuani S, Gili T, Bozzali M, Russo S, Porcari P, Cametti C, et al. Boronophenylalanine uptake in C6 glioma model is dramatically increased by L-DOPA preloading. Appl Radiat Isot. 2009;67(7-8 Suppl):S34-6.
7. Papaspyrou M, Feinendegen LE, Muller-Gartner HW. Preloading with L-tyrosine increases the uptake of boronophenylalanine in mouse melanoma cells. Cancer Res. 1994;54(24):6311-4.
8. Wittig A, Sauerwein WA, Coderre JA. Mechanisms of transport of p-borono-phenylalanine through the cell membrane in vitro. Radiat Res. 2000;153(2):173-80. 9. Hanaoka K, Watabe T, Naka S, Kanai Y, Ikeda H, Horitsugi G, et al. FBPA PET in boron neutron capture therapy for cancer: prediction of (10)B concentration in the tumor and normal tissue in a rat xenograft model. EJNMMI Res. 2014;4(1):70.
10. Delbeke D, Coleman RE, Guiberteau MJ, Brown ML, Royal HD, Siegel BA, et al. Procedure guideline for tumor imaging with 18F-FDG PET/CT 1.0. J Nucl Med. 2006;47(5):885-95.
11. Queiroz MA, Delso G, Wollenweber S, Deller T, Zeimpekis K, Huellner M, et al. Dose Optimization in TOF-PET/MR Compared to TOF-PET/CT. PLoS One. 2015;10(7):e0128842. 12. Zeimpekis K, Huellner M, De Galiza Barbosa F, Ter Voert E, Davison H, Delso G, et al. Clinical evaluation of PET image quality as a function of acquisition time in a new TOF-PET/MR compared to TOF-PET/CT - initial results. EJNMMI Phys. 2015;2(Suppl 1):A76.
13. Watanabe T, Hattori Y, Ohta Y, Ishimura M, Nakagawa Y, Sanada Y, et al. Comparison of the pharmacokinetics between L-BPA and L-FBPA using the same administration dose and protocol: a validation study for the theranostic approach using [(18)F]-L-FBPA positron emission tomography in boron neutron capture therapy. BMC Cancer. 2016;16(1):859.
Figures