2757
Brain morphometric and cellular metabolic alterations in patients with obsessive–compulsive disorder1National Institute of Biomedical Imaging and Bioengineering, National Institutes of Health, Bethesda, MD, United States, 2Radiology, Chonnam National University Medical School, Gwangju, Korea, Republic of
Synopsis
Obsessive–compulsive disorder (OCD) causes neural dysfunction associated with cognitive deficit and emotional dysregulation. To our knowledge, however, no one has applied the combined neuroimaging study of morphometric and metabolic brain abnormalities in patients with OCD. Therefore, this study assessed the associations of the gray matter (GM) and white matter (WM) volume alterations in conjunction with in vivo cellular metabolic changes in patients with OCD. Our findings will be helpful to aid us in the understanding of neurocognitive impairment in OCD, and thus, enhancing the diagnostic accuracy for OCD by additional information on the associated cerebral volume change and metabolic abnormality.
Purpose
Obsessive–compulsive disorder (OCD) causes neural dysfunction associated with cognitive deficit and emotional dysregulation. To our knowledge, however, no one has applied the combined neuroimaging study of morphometric and metabolic brain abnormalities in patients with OCD. Therefore, this study assessed the associations of the gray matter (GM) and white matter (WM) volume alterations in conjunction with in vivo cellular metabolic changes in patients with OCD.Methods
Thirty six right-handed subjects including 18 patients (mean age, 27.6±8.0 years) diagnosed with OCD by a psychiatrist using the DSM-IV-TR and 18 age-matched healthy controls (mean age, 30.7±7.5 years) underwent high-resolution T1-weighted magnetic resonance imaging (MRI) and proton magnetic resonance spectroscopy (1H-MRS) at 3 T Magnetom Verio MR scanner (Siemens Medical Solutions, Erlangen, Germany) with a birdcage head coil. The voxel localization of 1H-MRS was localized in the right DLPFC, which is considered more sensitive to OCD symptoms than left DLPFC, as well as one of the key centers associated with cognitive processing in OCD.
The MRI data were post-processed using the SPM12 program with DARTEL-based voxel-based morphometry (VBM) analysis. The MRIs were reconstructed using an optimized protocol. Alterations in GM and WM volumes in the patients with OCD and healthy controls were assessed by the independent two-sample t-test with multiple comparisons using family-wise error (FWE at p<0.05).
MR spectra were post-processed and analyzed using a MRS data analysis package (Siemens Medical Solutions). Seven major brain metabolites were assigned from the MR spectra as follows: Lip (0.91 ppm), lactate (Lac; 1.30 ppm), N-acetylaspartate (NAA; 2.02 ppm), creatine (Cr; 3.02 ppm), choline (Cho; 3.20 ppm), mI (3.56 ppm), β∙γ-glutamine/glutamate (Glx; 2.05-2.50 ppm), and α-Glx (3.65-3.80 ppm). The quantification of the brain metabolites was evaluated as the relative values to the Cr resonance at 3.02 ppm.
Also, the correlations of morphometric
changes with metabolic changes were analyzed by Pearson’s correlation test with
a 95% confidence interval.
Results and Discussion
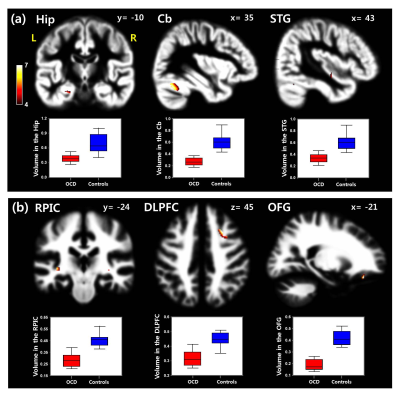
In voxel-based morphometry (VBM) with DARTEL algorithm, the patients showed significantly reduced GM volumes, especially in the cerebellum (Cb), hippocampus (Hip), and superior temporal gyrus, together with significantly reduced WM volumes in the retrolenticular part of the internal capsule, dorsolateral prefrontal cortex (DLPFC) and orbitofrontal gyrus (OFG) (Fig. 1).
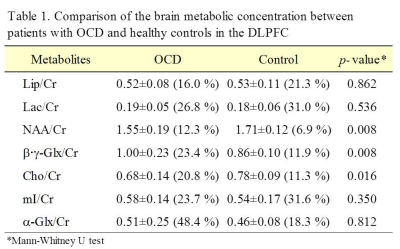
In 1H-MRS, the ratios of N-acetylaspartate/creatine (NAA/Cr) and choline (Cho)/Cr were significantly lower in the DLPFC of the patients than in the controls, whereas the ratio of β∙γ-glutamine-glutamate (β∙γ-Glx)/Cr was significantly higher in the patients than in the controls (Table 1).
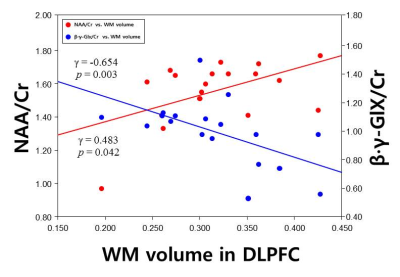
Interestingly, the WM volume of the DLPFC was positively correlated with the ratio of NAA/Cr (γ=0.483, p=0.042; Fig. 2), whereas the WM volume was negatively correlated with the ratio of β∙γ-Glx/Cr (γ=-0.654, p=0.003; Fig. 2).
Conclusion
Our study provides the first evidence for the association of the morphometric and in vivo metabolic abnormalities in OCD. The findings will be helpful to aid us in the understanding of neurocognitive impairment in OCD, and thus, enhancing the diagnostic accuracy for OCD by additional information on the associated cerebral volume change and metabolic abnormality.Acknowledgements
This work was supported by the funds from the National Research Foundation of Korea (2017R1A6A3A11030092; 2018R1A2B2006260) and JNU Research Distinguished Emeritus Professor (2017-2022).References
Woolley J, Heyman I, Brammer M, et al. Brain activation in paediatric obsessive compulsive disorder during tasks of inhibitory control. Br J Psychiatry 2008;192(1):25-31.Figures