2362
Serial ADC measurements in the T2 hyperintense, but otherwise normal-appearing white matter of glioblastoma patients correlates with survival1Department of Radiology, Na Homolce Hospital, Prague, Czech Republic, 2Department of Neurosurgery, Na Homolce Hospital, Prague, Czech Republic
Synopsis
Glioblastoma is the most common malignant primary intracranial tumor and, despite multi-modal treatment, the prognosis remains poor. Additional tools to improve early detection or evaluate treatment response are highly desirable. We evaluated serial ADC measurements in the T2-hyperintense, but otherwise normal-appearing white matter at 1.5 T in thirty-five subjects diagnosed with glioblastoma and treated by surgical resection, radiotherapy, temozolomide and tumor-treating fields. We found that serially increasing ADC in the T2-hyperintense, but otherwise normal-appearing white matter in glioblastoma patients is prognostically favorable, with significantly greater overall survival and progression-free survival in patients with increasing ADC.
INTRODUCTION
Glioblastoma (GBM) is the most common malignant primary intracranial tumor and, despite multi-modal treatment, the prognosis remains poor.1 Additional tools to improve early detection or evaluate treatment response are highly desirable, and quantitative MR parameters, including those derived from diffusion imaging, may advance our knowledge on the biological characteristics of gliomas both in diagnostic and treatment settings. Based on the positive results of a pilot study evaluating diffusion tenor imaging characteristics in the white matter near the resection cavity in 13 subjects with glioblastoma, we aimed to evaluate the prognostic value of diffusion restriction in a new, larger cohort of glioblastoma patients.METHODS
Thirty-five subjects diagnosed with glioblastoma were treated by surgical resection, radiotherapy, temozolomide and tumor-treating fields (TTFields).2 All subjects were followed by MRI at 1.5 T approximately every two months (total range 160-1810 days) with standard imaging, including diffusion-weighted imaging (DWI; b=1000 s/mm2), until tumor progression. Apparent diffusion coefficient (ADC) maps were calculated using FSL and freehand ROIs were placed on B0 images within the T2 hyperintense white matter (T2HWM) near the resection cavity by a single investigator (AMR), and then projected onto the ADC maps. Additionally, an ROI was similarly placed within the normal-appearing white matter (NAWM). Statistical analyses were performed in R. Final values used in the analyses (ADC-ratio) were obtained by dividing ADC in T2HWM by ADC in NAWM. Linear regression slopes (ADC-ratio vs. time) were fitted for individual subjects. We further explored ADC changes in a subgroup of 26 patients with DWI data available just prior to initiating, and for the first 180 days, of TTFields treatment; we transformed these initial data (ADC-ratio vs. time) to functional space by means of functional data analysis and further performed k-means clustering on the response functions, with the number of clusters determined by minimizing the Bayesian information criterion.RESULTS
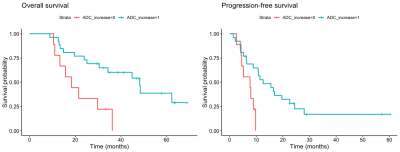
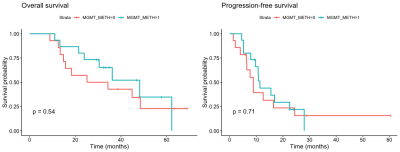
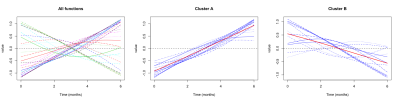
A positive slope was observed in ADC-ratio over treatment duration in 26 subjects, while in the remaining 9 subjects the slope was negative. We found a significant difference between subjects with positive and negative regression slopes in overall survival (OS; hazard ratio = 0.27 [0.1–0.69], log rank p = 0.009) and progression-free survival (PFS; hazard ratio = 0.31 [0.12–0.81], log rank p = 0.02), with positive regression slope associated with more favorable outcome. We did not detect any significant differences in OS (p=0.54) or PFS (p=0.71) with regard to MGMT methylation status. In exploring ADC-ratio changes within the first 180 days of TTFields treatment, 2 clusters were identified from all functions: in cluster “A” there was a mean positive slope (14 subjects), while in cluster “B” there was a mean negative slope (12 subjects). Using this classification (cluster A/B), no significant differences in OS (p=0.85) or PFS (p=0.75) were detected between the 2 subgroups. Initial positive ADC-ratio slope (cluster “A”) was good predictor of over-all positive slope covering the entire measurement period (accuracy 86%), while initial negative slope (cluster “B”) was no better than chance at predicting over-all slope covering the entire measurement period (accuracy 50%).DISCUSSION
Our data show that increasing ADC in the T2 hyperintense white matter of glioblastoma patients is favorable, with significantly greater OS and PFS in patients with increasing ADC over time. Changes in ACD likely reflect changes in tumor density in the affected white matter, with decreasing values (increasing diffusion restriction) corresponding to tumor progression. Although MGMT methylation is known to be favorable with respect to survival, no differences in OS or PFS were detected with regard to MGMT methylation status in our subjects. We further attempted to identify changes in ADC within the first 180 days of TTFields treatment as a likely reflection of early treatment response and we identified 2 clusters: subjects with positive changes (positive ADC slope), and subjects with negative changes (negative ADC slope). We did not detect any differences in OS or PFS between these 2 subgroups, likely due to the fact that a negative slope in the early treatment period was not predictive of the slope over the entire treatment period (accuracy: 50%). A positive slope in the early treatment period was however highly predictive of a positive slope over the entire treatment period (accuracy: 87%), and thus favorable survival outcomes. Therefore, treatment response is likely delayed in some subjects and declining ADC measurements in the early treatment period with TTFields does not necessarily indicate poor response or necessitate treatment termination.CONCLUSION
Serially increasing ADC in the T2-hyperintense, but otherwise normal-appearing white matter in glioblastoma patients is prognostically favorable, with significantly greater OS and PFS in patients with increasing ADC.Acknowledgements
No acknowledgement found.References
1. Johnson DR, O’Neill BP. Glioblastoma survival in the United States before and during the temozolomide era. J Neurooncol 2012;107(2):359-64.
2. Kirson ED, Dbaly V, Tovarys F, et al. Alternating electric fields arrest cell proliferation in animal tumor models and human brain tumors. Proc Natl Acad Sci USA 2007;104(24): 10152–10157.
Figures