1706
Improved, rapid fetal-brain localization and orientation detection for auto-slice prescription1Athinoula A. Martinos Center for Biomedical Imaging, Charlestown, MA, United States, 2Department of Radiology, Harvard Medical School, Boston, MA, United States, 3Fetal-Neonatal Neuroimaging and Developmental Science Center, Boston Children's Hospital, Boston, MA, United States, 4Electrical Engineering and Computer Science, Massachusetts Institute of Technology, Cambridge, MA, United States, 5Radiology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, United States, 6German Center for Neurodegenerative Diseases, Bonn, Germany, 7Institute for Medical Engineering and Science, Massachusetts Institute of Technology, Cambridge, MA, United States
Synopsis
MRI has become an invaluable tool for assessing the development of the fetal brain and can remove diagnostic doubt after routine ultrasound exams. Motion between slice prescription and acquisition, however, poses a challenge to obtaining images aligned with the standard anatomical planes, essential for evaluating morphometry. To address this, we recently presented automated slice prescription for fetal-brain MRI based on registration to a template. Here, we propose improved and fully automated fetal-brain orientation detection to advance both reliability and speed. The fast estimation is achieved by localizing the brain and eyes in an EPI scout using blob detection techniques.
Introduction
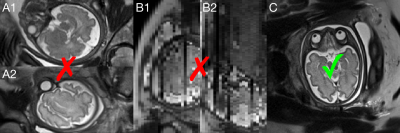
Fetal-brain MRI has become an invaluable tool for evaluating morphometric development and can remove diagnostic doubt after routine ultrasound exams.1,2 Motion between scan prescription and acquisition, however, frequently results in images with incorrect anatomical orientation. Typically, repeated acquisitions with manually corrected orientation are necessary to obtain views in the standard sagittal, coronal or axial planes, essential for assessing morphometry.3,4 Reslicing datasets is typically not viable as image quality of views across slices is dramatically reduced by through-plane motion (see Figure 1).5 These factors result in inefficient use of scan time due to discarded acquisitions.
To address this, we recently presented auto-slice prescription for fetal-brain MRI based on registration.6 Here, we advance this approach through improved fetal-brain orientation detection to increase reliability while being substantially faster. The fast update will reduce vulnerability to motion between prescription and acquisition. The orientation is derived by localizing the brain and eyes using maximally stable extremal regions (MSERs) – homogeneous-intensity blobs with steep transitions at their boundaries.7
Methods
Brain localization
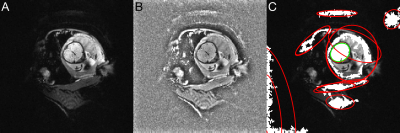
MSERs are derived from each slice of a 2D-EPI volume scout after removing non-uniformities by dividing by a smoothed version (see Figure 2). Potential non-brain MSERs are rejected using prior knowledge of biometry at corresponding gestational age (GA)8: center, size and shape of each MSER are estimated from an ellipse fit (see Figure 2C).9 MSERs far from the median center are removed before forming one median ellipse per slice. We estimate the brain center $$$B$$$ from the three largest of these.
Brain masking
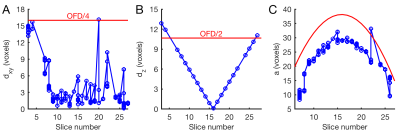
Local MSER search is performed after resampling at twice the resolution and enhancing edges by difference-of-Gaussians filtering. During outlier rejection the shape of the brain is considered by fitting a parabola to the distribution of major ellipse axes across slices (see Figure 3). The remaining MSERs are joined into a 3D mask.
Eye detection
Eye candidates are detected as MSERs in agreement with prior knowledge of ocular biometry.10 MSERs within one ocular diameter are clustered together. To identify the true eyes, we rank all pairs of clusters by their summed absolute deviation from prior knowledge, including binocular distance and cluster-brain distances.
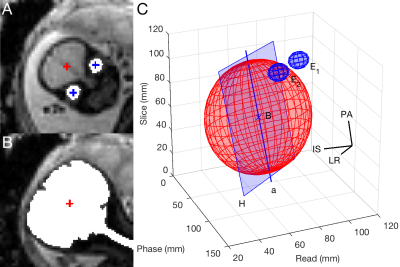
Orientation derivation
The left-right axis $$$LR$$$ passes through the eyes. We construct the posterior-anterior axis $$$PA$$$ from $$$B$$$ through the midpoint between the eyes. The inferior-superior axis $$$IS$$$ is perpendicular to $$$LR$$$ and $$$PA$$$. As $$$LR$$$ and $$$PA$$$ may not be strictly perpendicular, we form an orthonormal basis by replacing $$$LR$$$ with the cross product of $$$PA$$$ and $$$IS$$$.
To verify whether $$$LR$$$ and $$$IS$$$ may be flipped, we fit an ellipsoid to the brain mask and consider its major axis $$$a$$$ (see Figure 4): the plane $$$H$$$ containing $$$a$$$, parallel to $$$LR$$$, divides the brain into inferior and superior halves – the inferior part lies in the half space containing the eyes.
Results
Offline validation
Our algorithm was assessed in $$$n=21$$$ EPI acquisitions from fetuses at 26-38 weeks GA with oblique and double-oblique views. Brain and eyes were correctly detected in 86% of datasets despite variations in contrast and motion. Execution took ≤5 s per volume. Figure 5 shows a typical dataset resampled in the derived anatomical coordinates and illustrates how auto-slice prescription would have positioned the following scan. In case of erroneous key-point detection, the orientation was considerably off.
Deviation from manual localization
To quantify the accuracy of correctly detected key points we had a volunteer locate eyes and brain using FreeView/FreeSurfer11, and those sets of points were registered together.12 The maximum translational and rotational mismatch was 8.0 mm and 7.7°, respectively. Average deviations were (3.2±2.0) mm and (2.5±1.9)°.
Discussion
We demonstrated fully automated fetal-brain orientation detection for auto-slice prescription. Compared to registration6, using MSERs showed substantial improvement in reliability by 19 percentage points while reducing execution time threefold.
Discrepancies between automatic and manual key points were of the order of the voxel size (3 mm isotropic), due to between-slice motion and challenges in visually estimating the brain center from double-oblique views. For our purposes, however, only coarse alignment is needed.
Currently, technologists prescribe slices based on views of preceding ≤25-s scans.7 To reduce vulnerability to motion between prescription and acquisition, this delay can be more than halved by our auto-slice prescription combined with a ~5-s EPI scout. Further work may integrate the approach with motion correction, e.g. to automatically position low-resolution navigators13 on the fetal brain.
Conclusion
We present rapid, automated fetal-brain orientation detection using MSERs, with substantial improvement in reliability and execution time compared to registration-based approaches. The pipeline is suitable for automating on-scanner slice prescription.Acknowledgements
This research was supported by grants NINDS U01AG052564, NIBIB R01EB008547 and R01EB017337, NICHD R01HD085813 and 4R00HD074649.References
1. Pugash D, et al. Prenatal ultrasound and fetal MRI: the comparative value of each modality in prenatal diagnosis. Eur. J. Radiol. 2008;68(2):214–226.
2. Levine D, et al. Fetal central nervous system anomalies: MR imaging augments sonographic diagnosis. Radiology. 1997;204(3):635–642.
3. Saleem SN. Fetal MRI: An approach to practice: A review. J. Adv. Res. 2014;5(5):507–523.
4. Gholipour A, et al. Fetal MRI: A technical update with educational aspirations. Concepts Magn. Reson. Part A. 2014;43(6):237–266.
5. Malamateniou C, et al. Motion-compensation techniques in neonatal and fetal MR imaging. AJNR. Am. J. Neuroradiol. 2013;34(6):1124–1136.
6. M. Hoffmann, et al. Fast, automated slice prescription of standard anatomical planes for fetal brain MRI. Proc ISMRM, Paris, 2018.
7. Matas J, et al. Robust wide-baseline stereo from maximally stable extremal regions. Image Vis. Comput. 2004;22(10):761–767.
8. Snijders RJM, and Nicolaides KH. Fetal biometry at 14-40 weeks’ gestation. Ultrasound Obstet. Gynecol. 1994;4(1)34–48.
9. Keraudren K, et al. Automated fetal brain segmentation from 2D MRI slices for motion correction. Neuroimage. 2014;101:633–643.
10. Robinson AJ, et al. MRI of the fetal eyes: morphologic and biometric assessment for abnormal development with ultrasonographic and clinicopathologic correlation. Pediatr. Radiol. 2008;38(9):971–981.
11. Fischl B. FreeSurfer. Neuroimage. 2012;62(2):774–781.
12. Umeyama S. Least-Squares Estimation of Transformation Parameters between 2 Point Patterns. IEEE Trans. Pattern Anal. Mach. Intell. 1991;13(4):376–380.
13. Tisdall MD, et al. Prospective motion correction with volumetric navigators (vNavs) reduces the bias and variance in brain morphometry induced by subject motion. Neuroimage. 2016;127:11–22.
Figures