1115
Characterizing diffusion of myelin water in the living human brain using ultra-strong gradients and spiral readout1CUBRIC, School of Psychology, Cardiff University, Cardiff, United Kingdom
Synopsis
Myelin is a key white matter compartment, but myelin water is beyond the detection of conventional diffusion MRI methods because of its short T2. Here we combine ultra-strong gradients and spiral readout to achieve very short echo times (TE=30ms) at very high diffusion weighting (b=6000s/mm^2), with the aim of achieving significant sensitivity to the diffusion of myelin water in the living human brain. We investigated the challenge of disentangling 3 distinct compartments – including the short T2 component from myelin.
Introduction
Biophysical diffusion MRI (dMRI) models aim to characterize water diffusion within individual tissue-compartments. Myelin is a key white matter (WM) compartment that plays a critical role in information transport, and measuring myelin content is important for monitoring pathologies where demyelination, dysmyelination, or remyelination are implicated. However, myelin water is often considered ‘off-limits’ with typical dMRI measurements in the living human brain, because of its short transverse relaxation time (T2) and low volume fraction. Diffusion imaging of myelin water could potentially provide a more holistic characterization than alternative techniques1,2 currently allow, by also providing orientational information. Even though indirect sensitivity to myelin-water diffusion has been hypothesised through its interaction with other compartments3,4, direct characterisation of myelin water as a separate diffusion-compartment has thus far mostly been performed in excised tissue5,6 and simulations7. In this work, we exploit ultra-strong gradients and spiral readout to achieve very short echo times (TE=30$$$ms$$$) at very high diffusion weighting (b=6000$$$s/mm^2$$$), with the aim of achieving significant sensitivity to the diffusion of myelin water in the living human brain.Methods
In vivo human brain data
A pulsed-gradient-spin-echo (PGSE) sequence with spiral readout8 was implemented on a Siemens Connectom scanner with 300 mT/m gradients. dMRI
data from one healthy volunteer were acquired with b=[0,1000,2000,4000,6000]$$$s/mm^2$$$
and a range of TE’s, where the shortest TE was 5.5$$$ms$$$ for b=0$$$s/mm^2$$$, 22$$$ms$$$ for
b=1000$$$s/mm^2$$$ and 30ms for b=6000$$$s/mm^2$$$ (Fig. 1).
Simulations
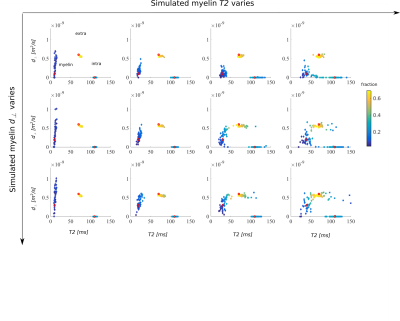
A commonly-used biophysical model with two compartments representing intra- and extra-axonal space (axially symmetric tensors with the former having zero perpendicular diffusivity)9,10 was extended to model compartment-specific T211, and an axially symmetric diffusion tensor was added representing the myelin compartment5. Here, the apparent perpendicular diffusivity includes contributions both from very slow diffusion orthogonal to the lipid bilayer, and faster diffusion circumferentially between layers. Signals were simulated using the in vivo MRI protocol, with a range of ground truth parameters (Fig.2) and Gaussian distributed noise (SNR=150 for b=0$$$s/mm^2$$$, TE=0$$$ms$$$).
Estimation
Parameter estimation was performed using the simplex algorithm12 with a cascaded fit where model complexity was increased in each cascade-step. The fit was initialised from multiple start positions, and the fit with the highest log-likelihood was selected.
Results
Simulations
The two-compartment diffusion model that served as the basis of the extended model proposed here is known to suffer from degeneracies, bias, and low precision13. Adding TE-dependency as an extra dimension has renewed hope for resolving these degeneracies11, and is essential for disentangling the myelin compartment. For the extended 3-pool diffusion-T2 model, Fig.2 studies degeneracies, bias, and precision of estimated signal fractions, apparent perpendicular diffusivities, and apparent T2. A low degree of dispersion was simulated using a Watson fiber orientation distribution (ODF, kappa=25). For low $$$d_{perp,m}$$$ (top row), increasing $$$T2_m$$$ initially increases precision of $$$d_{perp,m}$$$, but ultimately results in a lower discriminating power between $$$d_{perp,m}$$$ and $$$d_{perp,i}$$$. For larger $$$d_{perp,m}$$$ (bottom row), the clouds of solutions for myelin and the extra-axonal compartment start to overlap.
In vivo human brain data
Fig.3 shows results of the fitting of a 2-pool and 3-pool diffusion-T2 model. Including low TE-images achievable with the spiral acquisition into the fit results in a significantly lower T2-estimate for both pools (p=0.005 and p=7.7e-7), while diffusivities remain relatively similar. In agreement with the simulations, the clouds of solutions cannot be unambiguously distinguished, but the data supports the 3-pool over the 2-pool model in all voxels (evidenced by a lower AIC). A compartment with low T2 (<50$$$ms$$$) and low perpendicular diffusivity could be identified, which could indicate contributions from myelin water.
Discussion and Conclusion
We report on the ability to extract three distinct T2-diffusion species in the white matter of the living human brain. This has been facilitated by combining cutting edge hardware with robust spiral sampling of k-space, to drastically shorten TE. This access to a new measurement space (e.g. TE=30$$$ms$$$ for b=6000$$$s/mm^2$$$), gives a tantalising hint (Fig.3) that robustly quantifying the diffusivity of myelin water might be possible. However, it becomes apparent that more work needs to be done to get reliable quantification and to include factors such as exchange and dispersion. Exploring the cause of the dispersion in estimates is the subject of ongoing work, as well as the importance of stronger gradients/higher b-values/shorter TEs. Alternative solutions such as inversion recovery (IR) pulses could be used to suppress the long T1-component in WM, which is often assumed to arise from non-myelin water14. In the case of full suppression, the remaining signal could be represented by a single diffusion-T2 compartment, which should facilitate the fitting.Acknowledgements
CMWT is supported by a Rubicon grant (680-50-1527) from the Netherlands Organisation for Scientific Research (NWO) and Wellcome Trust grant (096646/Z/11/Z). The data were acquired at the UK National Facility for In Vivo MR Imaging of Human Tissue Microstructure funded by the EPSRC (grant EP/M029778/1), and The Wolfson Foundation. DKJ is supported by a Wellcome Trust Investigator Award (096646/Z/11/Z) and a Wellcome Trust Strategic Award (104943/Z/14/Z)References
1. MacKay A, Whittall K, Adler J, Li D, Paty D, Graeb D. In vivo visualization of myelin water in brain by magnetic resonance. Magnetic Resonance in Medicine. 1994;31(6):673–677.
2. Deoni SCL, Rutt BK, Arun T, Pierpaoli C, Jones DK. Gleaning multicomponent T1 and T2 information from steady-state imaging data. Magnetic Resonance in Medicine. 2008;60(6):1372–1387.
3. Jelescu IO, Zurek M, Winters K V., Veraart J, Rajaratnam A, Kim NS, Babb JS, Shepherd TM, Novikov DS, Kim SG, et al. In vivo quantification of demyelination and recovery using compartment-specific diffusion MRI metrics validated by electron microscopy. NeuroImage. 2016;132:104–114.
4. Lin M, He H, Tong Q, Ding Q, Yan X, Feiweier T, Zhong J. Effect of myelin water exchange on DTI-derived parameters in diffusion MRI: Elucidation of TE dependence. Magnetic Resonance in Medicine. 2018; 79(3):1650–1660.
5. Andrews TJ, Osborne MT, Does MD. Diffusion of myelin water. Magnetic Resonance in Medicine. 2006;56(2):381–385.
6. Stanisz GJ, Henkelman RM. Diffusional anisotropy ofT2 components in bovine optic nerve. Magnetic Resonance in Medicine. 1998;40(3):405–410.
7. Harkins KD, Does MD. Simulations on the influence of myelin water in diffusion-weighted imaging. Physics in Medicine and Biology. 2016
8. Li TQ, Kim DH, and Moseley ME. High-resolution diffusion-weighted imaging with interleaved variable-density spiral acquisitions. Journal of magnetic resonance imaging : JMRI, April 2005, 21:468-475
9. Jespersen, SN, Kroenke, CD, Ostergaard, L, Ackerman, JJ, Yablonskiy, DA. Modeling dendrite density from magnetic resonance diffusion measurements. Neuroimage 2007; 34 (4), 1473–1486.
10. Kroenke, CD, Ackerman, JJ, Yablonskiy, DA. On the nature of the NAA diffusion attenuated MR signal in the central nervous system. Magnetic Resonance in Medicine 2004; 52 (5), 1052–1059.
11. Veraart J, Novikov DS, Fieremans E. TE dependent Diffusion Imaging (TEdDI) distinguishes between compartmental T2 relaxation times. NeuroImage. 2018;182:360–369.
12. Press, William H., et al. Numerical recipes 3rd edition: The art of scientific computing. Cambridge university press, 2007.
13. Jelescu IO, Veraart J, Fieremans E, Novikov DS. Degeneracy in model parameter estimation for multi‐compartmental diffusion in neuronal tissue. NMR Biomed 2016; 29(1): 33-47.
14. Oh S-H, Bilello M, Schindler M, Markowitz CE, Detre JA, Lee J. Direct visualization of short transverse relaxation time component (ViSTa). NeuroImage. 2013;831500:485–492.
Figures