0981
Contrast Free Methods for Vascular Assessment in Lower Extremities of Diabetes1Washington University in St. Louis, Saint Louis, MO, United States, 2Radiology, Wayne State University, Detroit, MI, United States, 3The MRI Institute for Biomedical Research, Bingham, MI, United States
Synopsis
The purpose of this study is to develop a new contrast-free MR angiography technique without using any ECG triggering for the vascular assessment of lower extremities in patients with diabetes. Healthy volunteers and diabetes underwent both MR angiography and skeletal muscle perfusion imaging at rest and during an isometric contraction exercise. The angiography, perfusion, and even possible calcification of vessels can be assessed in one imaging session in patients with diabetes.
Objective
A hallmark of peripheral arterial disease (PAD) in the setting of diabetes, is the accumulation of densely calcified and occlusive disease of the tibial and pedal arteries. A radiation- and contrast-free imaging modality that can better characterize the extent of tibial and pedal arterial occlusive disease in patients with diabetes and/or PAD would provide great benefit to the diagnosis and treatment of this highly prevalent disease process. The objective of this ongoing study is to develop a new contrast-free-MR angiography (CF-MRA) technique without using any ECG signals and to integrate with existing skeletal muscle perfusion methods for the vascular assessment of lower extremities in patients with diabetes in one imaging session.Methods
CF-MRA technique The new CF-MRA allows simultaneous data collection for angiography, phase images, and susceptibility weighted imaging mapping (SWIM) with only approximately 5-min scan of the whole brain [1]. The sequence is a single 3D excitation interleaved rephrased/dephased 3-echo gradient-echo sequence (TE1/TE2/TE3 = 2.5/17.5/17.5 msec). By subtracting the flow-dephased images at TE3 from the flow-rephased images at TE2 with the same echo time, a MR angiogram (MRA) can be created. The SWIM data generated from the phase image of the short echo TE1 can be used to assess substances with high susceptibility values such as calcification and hemorrhage. Unlike other CF-MRA, the new CF-MRA does not need ECG triggering. This is an important feature for diabetes because ECG signal was not consistent in many individuals with diabetes who are overweight or obese, due to the increased subcutaneous fat and altered physiology, as well as prone to the interference by the strong magnetic field within a high field MRI system (≥ 3T).
MRA and MR perfusion in the lower extremities of diabetes We have performed a pilot study in 9 healthy volunteers (3 female, age: 61 ± 5 years; body-mass-index or BMI: 30.2 ± 7.7) and 9 age- and BMI-matched patients with diabetes and/or foot ulcers (3 female, age: 65 ± 11 years; BMI: 33.7 ± 7.3). All participants had ankle-brachial-index (ABI) and HbA1c tests prior to MRI exams. The MRI system was a 3 T trio or Prisma system (Siemens Healthcare, Erlangen, Germany). Each image session included MRA and perfusion imaging in one calf and/or one foot. The CF-MRA was performed only at rest and had an isotropic image resolution of 0.9 x 0.9 x 0.9 mm3. The scan time for 72-mm length of calf was 6 min 14 sec and for 63-mm length of foot was 4 min 15 sec. The perfusion measurements was performed at rest and during an isometric plantarflexion contraction within the MRI bore [2-3]. A contrast-free arterial spin labeling method was applied to obtain perfusion data [2]. Perfusion reserves were calculated from the ratio of exercise perfusion divided by the resting perfusion. One patient with diabetes and a relatively high ABI (> 1.4, non-compressible arteries due to calcification) was also evaluated for the SWIM to determine if there was any calcification in the calf vessels.
Results
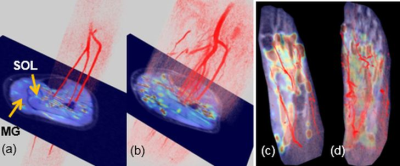
(1) The HbA1c was elevated in diabetes (7.7 ± 2.7) compared to healthy volunteers (5.4 ± 0.3, P = 0.1). Despite very similar ABI between healthy and diabetes, the perfusion reserves in two calf muscles (medial gastrocnemius and soleus) in diabetes was impaired (down 12-14%), compared to healthy volunteers (Figure 1).
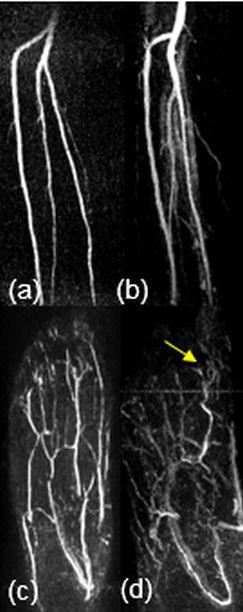
(2) No significant luminal stenosis (> 50%) was observed in all participants. Figure 2 shows two sets of CF-MRA images in a foot and calf of one healthy (left) and one patients (right) with diabetes and a foot ulcer (big toe). While the vessels in both calves appear normal, the vessels in the diabetic foot show more diffuse and less signals compared to the healthy foot.
(3) Figure 3 shows the 3D display of integrated exercise perfusion maps and CF-MRA in the same subjects in Figure 2. Although the calf perfusion map of the patients with diabetes appear normal, relatively reduced overall exercise perfusion was observed in the patient’s foot.
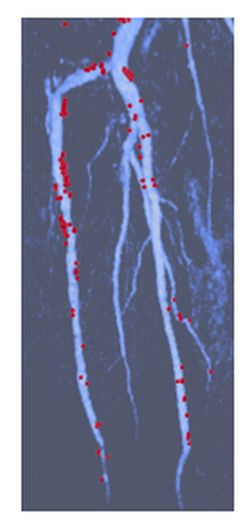
(4) Figure 4 shows a 3D display of calf vessels with several calcification segments (red) in the patient with diabetes and a high ABI, illustrating diffusive calcification on the anterior-tibial artery.
Discussion and conclusions
The ongoing pilot study demonstrates potentials of the new CF-MRA method for imaging arteries of lower extremities without using any ECG signals. Exercise perfusion distribution can be measured in the same imaging session, which is particularly important in patients with diabetes who are prone to peripheral arterial disease and perfusion deficit in their lower extremities. With the capability of simultaneous acquisitions of SWIM, calcification imaging in MRA could be explored in this cohort of patients who are prone to the calcified outflow arterial disease.Acknowledgements
This study was supported in part by research grants NIH R21 AR065672 and R01DK105322.References
1. Chen YS, Liu SF, Buch S, Hu JN, Kang Y, Haacke EM, Magn. Reson. Imaging, 2018, 47: 1 – 6.
2. Zheng J, An H, Coggan AR, Zhang X, Bashir A, Muccigrosso, D, Peterson LR, Gropler RJ. Magn Reson Med, 2014;71:318-325.
3. Edalati M, Hastings MK, Muccigrosso D, Sorensen CJ, Hildebolt C, Zayed M, Mueller MJ, Zheng J. J Mag Reson Imag, in press, 2019.
Figures