0195
Amid Proton Transfer-Weighted Imaging vs. Diffusion-Weighted Imaging vs. FDG-PET/CT: Capability for Management of Solitary Pulmonary Nodules1Division of Functional and Diagnostic Imaging Research, Department of Radiology, Kobe University Graduate School of Medicine, Kobe, Japan, 2Advanced Biomedical Imaging Research Center, Kobe University Graduate School of Medicine, Kobe, Japan, 3Canon Medical Systems Corporation, Otawara, Japan, 4Center for Radiology and Radiation Oncology, Kobe University Hospital, Kobe, Japan, 5Division of Radiology, Department of Radiology, Kobe University Graduate School of Medicine, Kobe, Japan
Synopsis
We hypothesized that APTw imaging had equal or better potential for diagnosis of SPNs and prediction of postoperative recurrence prediction in postoperative lung cancer patients, when compared with DWI and FDG-PET/CT. In addition, multiparametric approach among all three methods had better potential than single-parametric approach on each method in this setting. The purpose of this study was to compare the diagnosis and prediction capabilities of pulmonary nodules among single- and multi-parametric approaches by APTw imaging, DWI, and FDG-PET/CT.
Introduction
Differentiation of malignant from benign nodules and prediction of recurrence group from non-recurrence group in postoperative lung cancer patients are essential for radiological examination in routine clinical practice. Currently, CT and MR imaging including diffusion-weighted imaging (DWI) as well as dynamic contrast-enhanced MR imaging have been applied for morphological evaluation, although FDG-PET and PET/CT are applicable molecular imaging technique in various clinical and academic interest. As compared with FDG-PET or PET/CT, chemical exchange saturation transfer (CEST) imaging at 3.5 ppm (APT-weighted imaging: APTw imaging) has been suggested as the new technique for MR-based molecular imaging and reported as having the potential for diagnosis of thoracic lesions as well as pulmonary nodules (1, 2). However, no major reports have been reported the capability for differentiating malignant from benign solitary pulmonary nodules (SPNs) and recurrence from non-recurrence groups in candidates for surgical resection due to lung cancer among APTw imaging, DWI and PET/CT. We hypothesized that APTw imaging had equal or better potential for diagnosis of SPNs and prediction of postoperative recurrence prediction in postoperative lung cancer patients, when compared with DWI and FDG-PET/CT. In addition, multiparametric approach among all three methods had better potential than single-parametric approach on each method in this setting. The purpose of this study was to compare the diagnosis and prediction capabilities of pulmonary nodules among single- and multi-parametric approaches by APTw imaging, DWI, and FDG-PET/CT.Materials and Methods
113 consecutive patients (69 men, 44 women; mean age 71 years) with 122 pulmonary nodules prospectively underwent CEST imaging and DWI at 3T MR system (Vantage Titan 3T, Canon Medical Systems Corporation), FDG-PET/CT, pathological examinations from specimens obtained by transbronchial or CT-guided biopsies or surgical resection, treatment and/ or more than 2 years follow-up examinations. According to the pathological examination results, all nodules were divided into following two groups: malignant nodules (n=76) and benign pulmonary nodules (n=46). 67 out of 76 patients with malignant nodules were operated. Based on the results of follow up examination, 67 operated patients were divided as follows: non-recurrence group (n=52) and recurrence group (n=15). To obtain CEST data in each subject, respiratory-synchronized FASE imaging was conducted following a series of magnetization transfer (MT) pulses. Then, magnetization transfer ratio asymmetry (MTRasym) was calculated from z-spectra in each pixel, and MTRasym map was computationally generated. To obtain radiological indexes on CEST imaging, DWI and PET/CT, ROIs were placed over each lesion, and determined MTRasym, apparent diffusion coefficient (ADC) and maximum standard uptake value (SUVmax). Then, Student’s t-test was performed to determine the MTRasym, ADC and SUVmax between malignant and benign nodules and between recurrence and non-recurrence groups in operated patients. Multivariate logistic regression analysis was performed to investigate the discriminating factors of malignant from benign nodules and recurrence from non-recurrence groups. In addition, ROC analyses were also performed to differentiating each two groups. Finally, sensitivity, specificity and accuracy were compared each other by means of McNemar’s test. A p value less than 0.05 was considered as significant in this study.Results
Representative cases are shown in Figures 1 and 2. MTRasym, ADC and SUVmax had significant difference between malignant and benign SPNs (p<0.05) and between recurrence and non-recurrence groups (p<0.05). Multivariate regression analyses identified MTRasym (malignant vs. benign: Odds ratio [OR], 1.85, p<0.0001; recurrence vs. non-recurrence: 3.71, p=0.0008), ADC (malignant vs. benign: OR, 0.02; recurrence vs. non-recurrence: N/A, p=0.44) and SUVmax (malignant vs. benign: OR, 2.1, p=0.04; recurrence vs. non-recurrence: 5.8, p=0.009) as significant differentiators. Results of ROC analyses and diagnostic performance comparison are shown in Figure 3. For differentiating malignant from benign SPNs, area under the curves (AUCs) of MTRasym (AUC=0.88) and combined indexes (AUC=0.92) were significantly larger than that of SUVmax (Az=0.78, p<0.05). For distinguishing malignant from benign SPNs, sensitivities and accuracies of MTRasym, ADC and combined indexes were significantly higher than those of SUVmax (p<0.05). On postoperative recurrence prediction, specificity and accuracy of combined indexes were significantly higher than those of MTRasym and SUVmax (p<0.05).Conclusion
MTRasym, ADC and SUVmax were significant predictors for differentiating malignant from benign nodules, although MTRasym and SUVmax were significant predictors for distinguishing recurrence from non-recurrence groups. Multiparametric approaches of MRI and PET/CT have better potential than PET/CT alone in these settings, although APTw imaging and/ or DWI were also more accurate than PET/CT for diagnosis of pulmonary nodule.Acknowledgements
No acknowledgement found.References
1. Ohno Y, Yui M, Koyama H, et al. Radiology. 2016; 279(2): 578-589.
2. Ohno Y, Kishida Y, Seki S, et al. J Magn Reson Imaging. 2018; 47(4): 1013-1021.
Figures

Figure 1. 62-year-old female with invasive adenocarcinoma (L to R: thin-section CT, DWI, ADC map, MTRasym map fused with T2WI, and SUVmax map fused with CT)
Thin-section CT demonstrates a nodule with bubble like appearance in the right upper lobe. SUVmax of this nodule was 2.6. ADC was 1.05×10-3mm2/s. APTw image shows low MTRasym with the value of 1.25. This case was false-negative on PET/CT, and true-positive on DWI and APTw image. When combined both indexes, PET/CT with APTw image was also diagnosed as malignant nodule and determined as true-positive case.

Figure 2. 81-year-old male with invasive aspergilosis (L to R: thin-section CT, DWI, ADC map, MTRasym map fused with T2WI, and SUVmax map fused with CT)
Thin-section CT demonstrates a nodule with cavity in the right lower lobe. SUVmax of this nodule was 3.5. ADC was 1.28×10-3mm2/s. CEST image shows low MTRasym with the value of -1.57. This case was false-positive on PET/CT, and true-negative on DWI and CEST. When combined both indexes, PET/CT with CEST was also diagnosed as malignant nodule and determined as true-negative case.
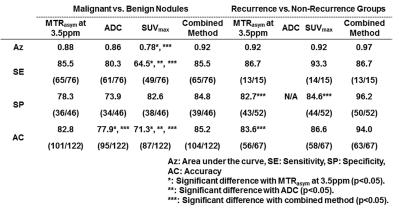
Figure 3. Comparison of diagnostic performance among MTRasym at 3.5ppm, ADC and SUVmax for distinguishing malignant and benign SPNs amd recurrence from non-recurrence groups in postoperative lung cancer patients.
Sensitivities and accuracies of MTRasym, ADC and combined indexes were significantly higher than those of SUVmax for distinguishing malignant from benign SPNs (p<0.05). In addition, specificity and accuracy of combined indexes were significantly higher than those of MTRasym and SUVmax on prediction of postoperative recurrence in lung cancer patients (p<0.05).