Lesion Detection (MS, Vascular Lesions)
1Radiology, UOEH School of Medicine, Japan
Synopsis
The role of brain MRI in diagnosis of multiple sclerosis (MS) and vascular lesions is well established, and the recently developed MR techniques, including synthetic MRI, myelin map with q-Space diffusion MRI, susceptibility-weighted imaging (SWI) and quantitative susceptibility mapping (QSM), further improve the diagnostic value in a research and clinical routine setting. This course will introduce the recent data pertaining to the use of new MR techniques in assessing MS lesion and small vascular lesions (cerebral microinfarcts).
Background
Conventional MRI parameters such as the number and distribution of focal T2 lesions and contrast-enhancing lesions are well established in diagnosis of multiple sclerosis (MS) lesions. However, these MRI parameters shows limited correlation with clinical outcome measures such as those measuring physical and cognitive decline (1). Moreover, although histopathologic studies suggest the presence of numerous cortical lesions in MS, the conventional MRI pulse sequences were found to largely miss these lesions and even with the use of newer MRI techniques such as 3D FLAIR or double inversion recovery (DIR), lesion detection remains suboptimal (2). Therefore, there is a crucial need for further MRI techniques focusing on more specific imaging markers in particular those related to neurodegenerative aspects of MS pathology. Similarly, detection of the chronic microinfarcts on conventional MRI would faces technical challenges in spatial resolution and in discrimination from other chronic lesions, such as white matter T2 hyperintensities, although a ssociation between microinfarcts and cognitive decline has been established by population-based pathological study (3).Purpose
This course will introduce the recent data pertaining to the use of new MR techniques in assessing MS lesion and microinfarcts.Method
The MRI assessments have been applied to clinical in the following areas:
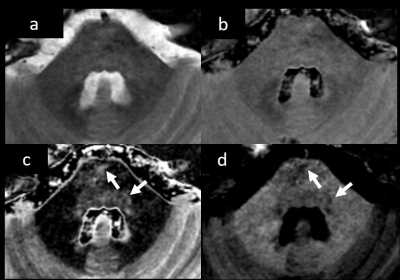
- Synthetic MRI - Synthetic MRI enables the creation of various contrast-weighted images including phase-sensitive inversion recovery (PSIR) and 2 types of double inversion recovery (DIR) with white matter attenuated inversion recovery (WAIR) and gray matter attenuated inversion recovery (GAIR) from a single MR imaging quantification scan, which has the potential to be useful for detecting MS plaques (4) (Fig 1).
- Myelin map - Myelin map with q-Space diffusion MRI (QSI) is practical for visualizing white matter and is sensitive enough to depict dysmyelination, demyelination, and remyelination in MS patients (5). Phase difference enhanced imaging (PADRE) - The phase-weighted MRI technique “PADRE” can delineate the gray matter (GM) and white matter (WM) clearly due to the difference in myelin concentration, which is useful for detecting GM involvement of the juxtacortical MS lesions (6).
- Quantitative susceptibility mapping (QSM) - MR imaging with QSM increases the sensitivity in cortical MS lesion detection (increased susceptibility as the consequence of iron content) and improves distinction between juxtacortical and mixed WM-GM lesions (7). The QSM can also detect MS-related tissue changes in the basal ganglia at the earliest stage of the disease (8). Furthermore, on QSM, we can detect pathophysiologic features of MS lesions (9); magnetic susceptibility of MS lesions increases as it changes from enhanced to nonenhanced phase, and it gradually dissipates back to susceptibility similar to that of normal white matter (10), suggesting that QSM may be an imaging biomarker for monitoring MS lesion activities.
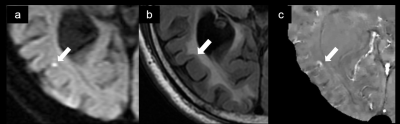
- MRI assessment of cerebral microinfarcts – Recently, in vivo detection of microinfarcts is possible using MRI; the cortical microinfarcts could be detected in 6% of elderly people at high-resolution 3T MRI (11). However, main limitation of previous MRI studies (12,13) is to perform in patients with no history of stroke or months to years after stroke, at a time when the infarct has undergone significant reorganization using only T2WI and FLAIR. Therefore, exact definition or finding of microinfarcts for MRI are still under discussion, because there is no proof of the nature of the microinfarcts (no confirmation during acute phase of the microinfarcts). We will present the evolution of DWI-positive acute microinfarct on follow-up MRI, including synthetic MRI, susceptibility-weighted imaging (SWI), and QSM (Fig 2).
Acknowledgements
No acknowledgement found.References
1. Wattjes M, Steenwijk M, Stangel M. MRI in the diagnosis and monitoring of multiple sclerosis: an update. Clinical neuroradiology 2015;25(2):157-165.
2. Seewann A, Kooi E-J, Roosendaal S, et al. Postmortem verification of MS cortical lesion detection with 3D DIR. Neurology 2012;78(5):302-308.
3. Smith EE, Schneider JA, Wardlaw JM, Greenberg SM. Cerebral microinfarcts: the invisible lesions. The Lancet Neurology 2012;11(3):272-282.
4. Hagiwara A, Hori M, Yokoyama K, et al. Synthetic MRI in the detection of multiple sclerosis plaques. American Journal of Neuroradiology 2017;38(2):257-263.
5. Fujiyoshi K, Hikishima K, Nakahara J, et al. Application of q-space diffusion MRI for the visualization of white matter. Journal of Neuroscience 2016;36(9):2796-2808.
6. Futatsuya K, Kakeda S, Yoneda T, et al. Juxtacortical lesions in multiple sclerosis: Assessment of gray matter involvement using phase difference-enhanced imaging (PADRE). Magnetic Resonance in Medical Sciences 2016;15(4):349-354.
7. Kakeda S, Futatsuya K, Ide S, et al. Improved detection of cortical gray matter involvement in multiple sclerosis with quantitative susceptibility mapping. Academic radiology 2015;22(11):1427-1432. 8. Langkammer C, Liu T, Khalil M, et al. Quantitative susceptibility mapping in multiple sclerosis. Radiology 2013;267(2):551-559.
9. Zhang Y, Gauthier SA, Gupta A, et al. Longitudinal change in magnetic susceptibility of new enhanced multiple sclerosis (MS) lesions measured on serial quantitative susceptibility mapping (QSM). Journal of Magnetic Resonance Imaging 2016;44(2):426-432.
10. Chen W, Gauthier SA, Gupta A, et al. Quantitative susceptibility mapping of multiple sclerosis lesions at various ages. Radiology 2014;271(1):183-192.
11. van Dalen JW, Scuric EE, van Veluw SJ, et al. Cortical microinfarcts detected in vivo on 3 Tesla MRI clinical and radiological correlates. Stroke 2015;46(1):255-257.
12. van Veluw SJ, Zwanenburg JJ, Engelen-Lee J, et al. In vivo detection of cerebral cortical microinfarcts with high-resolution 7T MRI. Journal of Cerebral Blood Flow & Metabolism 2013;33(3):322-329.
13. Brundel M, Reijmer YD, van Veluw SJ, et al. Cerebral microvascular lesions on high-resolution 7-tesla MRI in patients with type 2 diabetes. Diabetes 2014;63(10):3523-3529.
Figures