Introduction: Concurrent MR Imaging of Real-Time Event
1Brigham and Women's Hospital, Harvard Medical School, United States
Synopsis
The expression 'concurrent MRI' relates to the use of an MR scanner as part of a larger integrated system, as opposed to a standalone diagnostic tool. Examples include image-guided therapies and hybrid imaging, where changes to tissues can be induced and tracked in real time. In this session, the ability of MRI to capture changes caused by ultrasound energy deposition, radiation therapy, brain plasticity and catheter steering will be presented. In the present talk, our work on hybrid ultrasound+MR imaging and on MR-compatible sensor development will also be detailed.
Outcome/objectives:
Participants will be introduced to the field of concurrent MRI, whereby the MRI scanner is part of a larger integrated system rather than a standalone tool.Purpose:
The word ‘concurrent’ means ‘operating or occurring at the same time’ (Merriam-Webster Dictionary). Most commonly, MR imaging is performed on its own, for diagnostic purposes. But increasingly often it is performed instead as part of a greater integrated system, whereby the MR scanner operates in synchrony and in a complementary fashion with other devices. A variety of such integrated systems that employ MRI as one of its key components will be presented in this session. While part of the integrated system may cause changes in tissues, another part of the system may aim at tracking these changes in real time.
For example, MRI can be employed as a guidance system during therapy. High-intensity beams of ultrasound energy can be generated and properly focused to ablate targeted tissues [1-5], or to temporarily disrupt the lining of blood vessels and locally open the blood-brain barrier, to enable drug delivery [6,7]. Replacing the ultrasound energy by radiation as the destructive agent, MR guidance can also be applied to radiation therapy [8]; with the recent introduction of commercial MR-linac systems, the use of MRI for radiation therapy guidance may well flourish in the coming years. Elaborate catheter designs can function in synergy with the MRI equipment, whereby the catheter participates in the imaging process and the magnetic field of the MR scanner participates in steering the catheter [9]. MRI can even be employed to capture brain changes that occur as part of learning and experience, changes that are made possible by the plasticity of the brain [10].
In our own work, we developed ultrasound-based sensors that can accompany the patient into the MRI bore and provide a stream of high-temporal resolution information concurrent with the MR data acquisition [11-14]. Our vision is that in the future, many sensors of various types may collect information regarding scanner operation and patient behavior during the MR acquisition, and these diversified data will be input into machine learning algorithms for the reconstruction of higher-quality MR images.
Methods:
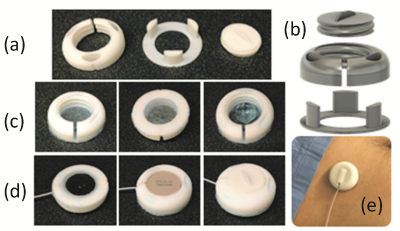
One of our ultrasound-based sensors, called ‘organ configuration motion’ (OCM) sensors, is shown in Fig. 1. A plastic capsule was designed and 3D-printed to accommodate the transducer and ultrasound gel. One side of the sensor is closed by a thin membrane essentially transparent to ultrasound energy but able to contain the gel. The sensor is fixed to the skin, and closed by twisting a lid that pushes the transducer onto the skin to achieve proper acoustic coupling. The sensors are compact, about 3x3x1 cm in size, and a multiplexing device was developed to allow up to four sensors to be used at a time. Application to the skin simply involved peeling a protective layer and pressing the device onto the appropriate site: the abdomen for monitoring respiratory motion, or the chest for cardiac gating. Further devices were developed to keep OCM and MRI data streams in sync, by detecting RF pulses from the MR scanner and firing the OCM sensor(s) in synchrony with these RF pulses [15]. Machine learning algorithms were developed to interpret signals and reconstruct images from the hybrid streams of OCM+MRI data that were obtained as a result.Results:
Up to now, hybrid OCM+MRI acquisitions have been used mostly to: help improve the temporal resolution of real-time MRI by up to two orders of magnitude [11-14]; to help detect cardiac activity even at high field strength, when magnetohydrodynamic effects can make electrocardiograms (ECGs) unreliable [12,16]; and to help handle breathing motion during MR thermometry and thermal ablation [17].Conclusion:
The main value of concurrent MRI is that it extends the modality beyond its usual role as a standalone diagnostic tool. As part of more complex integrated systems, MRI can play a key role in enabling therapeutic and hybrid imaging functionalities well beyond its standalone capabilities.Acknowledgements
Financial support from NIH grants R01CA149342, P41EB015898 and R03EB025546 is duly acknowledged. The content is solely the responsibility of the authors and does not necessarily represents the official views of the NIH.
References
[1] Elias WJ, Lipsman N, Ondo WG, Ghanouni P, Kim YG, et al. A randomized trial of focused ultrasound thalamotomy for essential tremor. N Engl J Med 2016;375(8):730-9.
[2] Aubry JF, Pauly KB, Moonen CT, Haar GT, Ries M, et al. The road to clinical use of high-intensity focused ultrasound for liver cancer: technical and clinical consensus. J Ther Ultrasound 2013;1:13.
[3] Hynynen K, Darkazanli A, Unger E, Schenck JF. MRI‐guided noninvasive ultrasound surgery. Med Phys 1993;20(1):107-15.
[4] de Senneville BD, Moonen CT, Ries M. MRI-guided HIFU methods for the ablation of liver and renal cancers. Therapeutic Ultrasound 2016:43-63.
[5] Quesson B, de Zwart JA, Moonen CT. Magnetic resonance temperature imaging for guidance of thermotherapy. J Magn Reson Imag 2000;12(4):525-33.
[6] Hynynen K, McDannold N, Vykhodtseva N, Jolesz FA. Noninvasive MR imaging-guided focal opening of the blood-brain barrier in rabbits. Radiology 2001;220(3):640-6.
[7] Treat LH, McDannold N, Vykhodtseva N, Zhang Y, Tam K, Hynynen K. Targeted delivery of doxorubicin to the rat brain at therapeutic levels using MRI‐guided focused ultrasound. International Journal of Cancer 2007;121(4):901-7.
[8] Stemkens B, Tijssen RH, de Senneville BD, Lagendijk JJ, van den Berg CA. Image-driven, model-based 3D abdominal motion estimation for MR-guided radiotherapy. Phys Med Biol 2016;61(14):5335-55.
[9] Wilson MW, Martin AB, Lillaney P, Losey AD, Yee EJ, Bernhardt A, Malba V, Evans L, Sincic R, Saeed M, Arenson RL, Hetts SW. Magnetic catheter manipulation in the interventional MRI environment. J Vasc Interv Radiol 2013;24(6):885-91.
[10] Zatorre RJ, Fields RD, Johansen-Berg H. Plasticity in gray and white: neuroimaging changes in brain structure during learning. Nature Neuroscience 2012; 15(4): 528-36.
[11] Preiswerk F, Toews M, Cheng C-C, Chiou Jr-G, Mei C-S, Schaefer LF, Hoge WS, Schwartz BM, Panych LP, Madore B. Hybrid MRI ultrasound acquisitions, and scannerless real-time imaging. Magn Reson Med 2017;78(3):897-908.
[12] Madore B, Cheng C-C, Preiswerk F. Ultrasound-based sensors for physiological motion monitoring. Session on ‘Does motion still Matter? New methods for handling motion’, 08:15 Thursday June 21st, ISMRM 2018, Paris, France.
[13] Preiswerk F, Toews M, Hoge WS, Chiou J-yG, Panych LP, Wells III WM, Madore B. Hybrid Utrasound and MRI Acquisitions for High-Speed Imaging of Respiratory Organ Motion. In: Navab N, Hornegger J, Wells W, Frangi A, editors. Medical Image Computing and Computer-Assisted Intervention – MICCAI 2015: Springer International Publishing, 2015:315-322.
[14] Preiswerk F, Toews M, Cheng C-C, Chiou Jr-y, Mei C-S, et al. Hybrid MRI-ultrasound acquisitions, and scannerless real-time imaging. ISMRM 2017, Honolulu, USA: p. 0033.
[15] Preiswerk F, Cai J, Cheng C-C, Hoge WS, Wu P-H, Panych LP, Madore B. RF-Sensing for Trigger-Based Synchronization of Auxiliary Devices, and Pulse-Sequence Debugging. ISMRM 2017, Honolulu, USA: p. 4444.
[16] Preiswerk F, Cheng C-C, Wu P-H, Panych LP, Madore B. Ultrasound-based cardiac gating for MRI. ISMRM 2017, Honolulu, USA: p. 4443.
[17] Wu P-H, Cheng C-C, Preiswerk F, Madore B. Application of hybrid MR-ultrasound imaging to multi-baseline thermometry. Session on ‘MRI guided interventions’, 13:45 Monday June 18th, ISMRM 2018, Paris France.
Figures