Bioeffects & Hazards from Static Field, Gradient, & RF Exposures
1Philips Healthcare, Netherlands
Synopsis
This talk provides an overview of the MR safety risks and its scientific background
Introduction
Diagnostic medical imaging is considered safe for patients and staff, especially when using non-ionizing radiationsuch as ultrasound and MRI. More than 4 million patients per month are subject to an MRI examination, with anestimated serious adverse event reporting rate (from FDA’s MAUDE database) of approx. 5 ppm. This means,nonetheless, that more than 250 humans are injured by a procedure that is intended for a harmless diagnosis.
A wealth of reviews on MRI safety can be found, see for example [1], [2] and [3], as well as (on-line) instruction [4],and training materials. It is essential to be aware of MRI related safety risks, and implement a safety program whenoperating MRI systems. Basic safety of MR systems is provided by implementation of the requirements of IEC60601-2-33 [5], the international safety standard developed and maintained by IEC and stakeholders. Otherdevices and equipment used in the vicinity of the MR system must be tested and clearly labelled as MR unsafe,safe, or conditional per IEC 62570 [6]. The relatively low number of incidents can only be realized by closecollaboration and strict vigilance of all stakeholders.
This talk will review the hazards associated with MRI, and consider three categories: constructional andoperational hazards, instantaneous biophysical effects, and potential long-term effects. An overview of causes,effects, and harm is given in Figure 1. Biological contamination and other hazards in the hospital environment(such as falling incidents, and patient data mix-up) are not covered in this presentation.
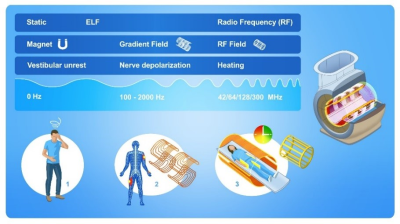
Causes of Direct Harm
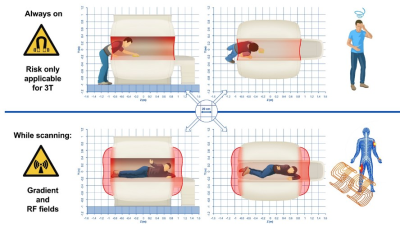
The principle of operation of the MRI system requires exposure of the patient to a strong static magnetic field,rapidly switching magnetic encoding fields, and intense pulsed radiofrequency fields. Interaction of these fieldswith the human body is discussed in the next section. The design of the MRI system also introduces direct hazardsinherent to the imaging process (attraction events, patient positioning, acoustic noise, and Helium exhaust) andarising from electro-magnetic interactions with RF coils (heating) and devices required for the medical procedure(malfunction).Attraction events
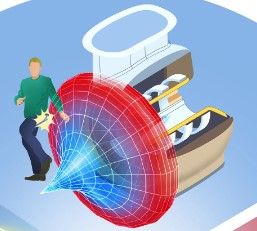
The strong magnetic field of actively-shielded MRI magnets decays rapidly, inside the MR shielded room. The high gradient of the magnetic field near the system (< 1 m outside the covers) imposes a very strong force on ferromagnetic objects. This magnetic force should be considered to “turn on suddenly”, and there is practically no possibility to withdraw from its influence once it engages with an object. Figure 2 provides a visual representation of this localized attraction hazard.
All objects for use near the MRI system must be tested and labelled for safety. Fatal events have been reported due to attraction of oxygen bottles; cleaning devices, fire extinguishers, hospital beds and wheel chairs can be equally dangerous.
Patient positioning
The magnet field-of-view being limited, imaging (extended) anatomy requires movement of the patient throughthe magnet. The patient couch is designed to prevent entrapment of body parts, but a sizeable amount of patientsexperience claustrophobia or similar anxiety. Careful preparation of the patient is required to help prevent anymechanical hazards, potentially leading to broken fingers.Acoustic noise
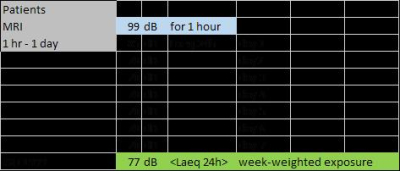
Spatial encoding magnetic fields are generated by rapidly changing currents in the gradient coils. These strong currents in the strong magnetic field impose Lorenz forces on the conductors, similar to the operation of music speakers. The possibility to vibrate is generally minimized by a structural stiff design. The dimensions of the gradient coil determine the resonance frequencies, which by design have a very high Q-factor. MRI sequences excite the frequency spectrum at primary frequencies < 1200 Hz, typically. Excitation at frequencies < 400 Hz is not “efficient” due to the mechanical characteristics of the gradient coil. Thus, most of the acoustic noise is generated between 400 and 1200 Hz. Avoiding sequences that drive resonance frequencies of the gradient coil can be very effective to reduce the acoustic burden of MRI. Nevertheless, appropriately applied hearing protection is required to provide approx. 25-30 dBA reduction of emitted sound pressure levels. MRI manufacturers use the NEMA MS-4 [7] standard procedure to characterize (worst case) acoustic emissions, expressed as equivalent to a 1 hour exposure (LA,eq-1h). MRI examinations generally do not extend this 1 hour exposure duration, and will not be repeated within 1 week for the same patient. Under these assumptions, IEC 60601-2-33 allows for 99 dBA at the ear (assuming sufficient and adequate hearing protection to reduce the system emission to the ear exposure level). The 99 dBA level can be understood when considering that an average exposure of 80 dBA over a week is considered acceptable by acoustic experts, and a single 1 hour exposure can be averaged over the week by the formalism provided in ISO 1999 [8]. An example of such calculation is provided in Table 1.
Acknowledgements
No acknowledgement found.References
No reference found.Figures