5661
Do you suffer from long-term memory loss? I don't remember...: An MRI pictorial review of neurodegenerative diseases1Radiology, Ng Teng Fong General Hospital, Singapore, Singapore, 2Diagnostic & Interventional Imaging, KK Women's & Children's Hospital, Singapore, Singapore
Synopsis
Neurodegenerative diseases are a large group of conditions with progressive, but variable, neurological deterioration over time. Dementia is a hallmark in many of these diseases. Classification using clinical phenotypes is suboptimal due to broad overlap in clinical manifestations, and recent approaches have favoured using neuropathological and biochemical criteria instead.
Neuroimaging using magnetic resonance imaging (MRI) has good correlation with the neuropathological classification, and can be used to aid the clinician in making an accurate diagnosis. This education exhibit provides an MRI pictorial review of the neurodegenerative diseases which are more common, and/or are more clearly defined from a neuropathological standpoint.
Introduction
Neurodegenerative diseases encompass a very large group of conditions with progressive, but variable, neurological deterioration over time. Dementia is a hallmark in many of these diseases. Attempts have been made to classify these conditions by clinical phenotype, but this has proven difficult as there is a broad overlap in clinical manifestations between various diseases. In addition, many conditions may already be far advanced by the time they are clinically distinct and are hence, past the window for useful intervention or treatment trials.
A useful classification system, based on neuropathological findings, has been proposed1,2. This broadly divides neurodegenerative diseases into conditions that result in abnormal deposition of tau proteins (the 'tauopathies'), those that have intracellular accumulation of alpha-synuclein (the 'synucleinopathies'), and other diseases with unique histological and biochemical abnormalities (e.g., cerebral amyloidosis, Huntington disease and the prion diseases).
This classification system also has the advantage of good correlation with specific neuroimaging findings on magnetic resonance imaging (MRI), which can help the clinician in clinching the correct diagnosis and intervening early. It also obviates the need for histological confirmation. This educational exhibit will provide a pictorial review of the typical MRI findings of the neurodegenerative diseases listed below, based on this neuropathological classification.
Tauopathies
These conditions result in the abnormal metabolism of microtubule associated tau proteins, leading to intracellular accumulation and formation of neurofibrillary tangles. Clinically, dementia is a hallmark and tends to occur early in the clinical course3. The specific entities are:
1. Alzheimer disease and its variants.
2. Frontotemporal dementia (Pick's disease), in which the abnormal protein involved is commonly tau protein, and less commonly TDP-43 (transactive response DNA binding protein 43 kDa). There are five clinical phenotypes with distinct MRI features4-6, namely:
a) Behavioural-variant frontotemporal dementia.
b) Semantic variant primary progressive aphasia (previously known as semantic dementia).
c) Nonfluent/agrammatic variant primary progressive aphasia (previously known as nonfluent aphasia).
d) Logopaenic variant primary progressive aphasia.
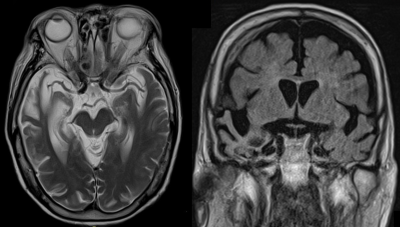
e) Right temporal variant frontotemporal dementia (see Fig. 1).
3. Corticobasal degeneration.
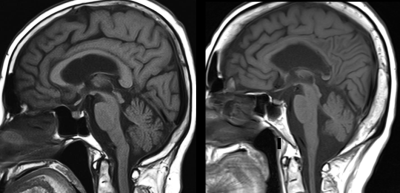
4. Progressive supranuclear palsy (see Fig. 2).
Synucleinopathies
Synucleinopathies are the result of impaired metabolism of the synaptic protein, alpha-synuclein, which then accumulates within neurons. There is considerable overlap in the clinical patterns of disease, and dementia is not a hallmark in all of the conditions. However, MRI features are typical and can help to differentiate between them7. They can be broadly separated into diseases that manifest intracellular Lewy bodies, and the multiple system atrophies, which do not:
1. Diseases with Lewy bodies:
a) Parkinson disease.
b) Dementia with Lewy bodies.
2. Multiple system atrophies:
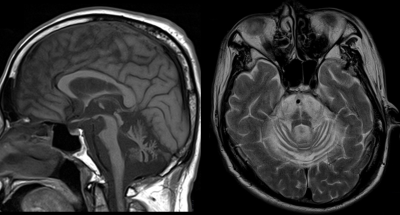
a) Cerebellar multiple system atrophy (MSA-C) (see Fig. 3).
b) Extrapyramidal (Parkinsonism-type) multiple system atrophy (MSA-P).
Other Neurodegenerative Diseases
The neurodegenerative diseases below are a clinically heterogeneous group that nonetheless, have clearly elucidated histological, biochemical and neuroimaging findings1,8:
1. Vascular cerebral amyloidosis, which includes:
a) Cerebral amyloid angiopathy.
b) Transthyretine-associated cerebral amyloidosis.
c) Neuronal intranuclear hyaline inclusion disease.
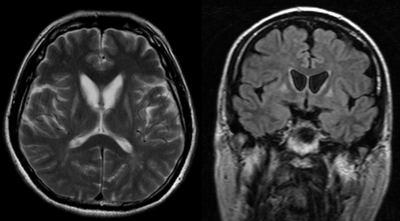
2. Huntington disease (see Fig. 4).
3. Prion diseases.
4. Amytrophic lateral sclerosis.
Acknowledgements
No acknowledgement found.References
1. Kovacs GG. Molecular Pathological Classification of Neurodegenerative Diseases: Turning towards Precision Medicine. Int J Mol Sci. 2016 Feb 2;17(2). pii: E189.
2. Dickson DW. Neuropathology of non-Alzheimer degenerative disorders. Int J Clin Exp Pathol. 2009 Aug 25;3(1):1-23.
3. Williams DR. Tauopathies: classification and clinical update on neurodegenerative diseases associated with microtubule-associated protein tau. Intern Med J. 2006 Oct;36(10):652-60.
4. Bott NT, Radke A, Stephens ML, Kramer JH. Frontotemporal dementia: diagnosis, deficits and management. Neurodegener Dis Manag. 2014;4(6):439-54.
5. Chare L, Hodges JR, Leyton CE, et al. New criteria for frontotemporal dementia syndromes: clinical and pathological diagnostic implications. J Neurol Neurosurg Psychiatry. 2014 Aug;85(8):865-70.
6. Josephs KA, Whitwell JL, Knopman DS, et al. Two distinct subtypes of right temporal variant frontotemporal dementia. Neurology. 2009;73(18):1443-50.
7. Brooks DJ, Tambasco N. Imaging synucleinopathies. Mov Disord. 2016 Jun;31(6):814-29.
8. Risacher SL, Saykin AJ. Neuroimaging Biomarkers of Neurodegenerative Diseases and Dementia. Semin Neurol. 2013 Sep;33(4):386-416.
Figures