5590
Clinical Validation of a Semiautomated Workflow for MR Elastography1Radiology, Mayo Clinic, Rochester, MN, United States
Synopsis
Magnetic Resonance Elastography (MRE) is a validated method for staging hepatic fibrosis utilizing MR images of acoustic wave propagation in the liver to measure hepatic stiffness. A new MRE analysis workflow, called ALEC, in which readers are presented with preliminary, automatically generated, ROIs was validated in a clinical environment using 1347 exams. The workflow failed in <1% of cases. Manual modification was performed on 18% of the exams, leading to a stiffness change of only 1% on average. The ALEC-assisted stiffness measurement workflow offers a faster and more reproducible way to perform MRE.
Introduction
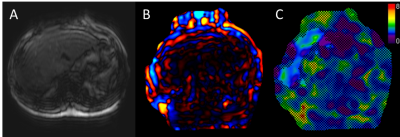
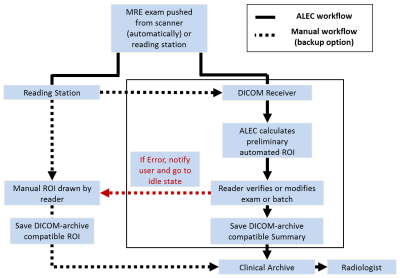
Magnetic Resonance Elastography (MRE) is a noninvasive, quantitative method for diagnosing hepatic fibrosis.1 It uses MR images of acoustic wave propagation in the liver to produce quantitative tissue stiffness images (elastograms). MRE magnitude, wave, and stiffness images (Figure 1) are analyzed to select an artifact-free ROI from which to report the liver stiffness that is used in diagnosis. A fully automated method for selecting ROIs, called ALEC,2 has been developed and validated at our institution, and showed a higher agreement with an expert reader than did clinical, MRE-trained technicians. In September 2015, our institution’s clinical practice was switched to a semiautomated workflow in which all MRE exams are pushed to ALEC, a preliminary automated ROI is generated, an MRE-experienced technician reviews or modifies it, and then pushes the report to the DICOM archive (PACS) (Figure 2). The purpose of this study was to retrospectively review and validate this workflow.Methods
All exams processed by ALEC from January to October 2017 were retrospectively reviewed for this study. The exams were acquired with various GRE and SE-EPI MRE sequences on 1.5T and 3T GE (Waukesha, WI) scanners. The ROIs and stiffnesses from exams with reader-modified ROIs were compared to their original, fully automated counterparts. The automatically generated ROI was considered a failure if (1) after the modification the ROI the stiffness changed by more than 10%, or (2) if more than 5% of the original ROI contained nonliver tissue or artifacts that affected the elastograms. Exams with processing errors recorded on the ALEC station were reviewed to determine if the error resulted from ALEC-related issues or another source.Results
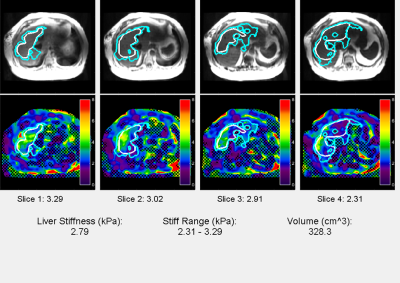
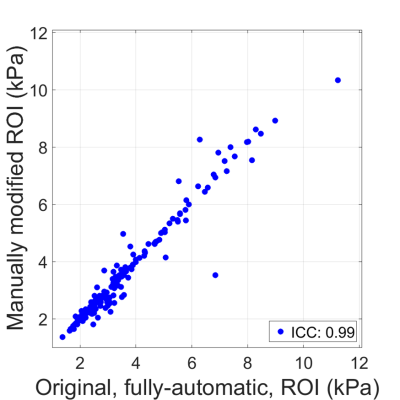
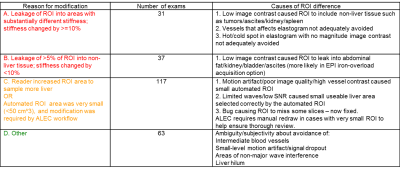
An example of an ALEC report is shown in Figure 3. A total of 1347 patient MRE exams were processed with ALEC during the 9-month validation period and each case was reviewed by one of 8 MRE-trained technicians. Modifications to the preliminary automated ROIs were performed in one or more slices in 248 exams (18%). The reported liver stiffness changed by 1% on average and the intraclass correlation coefficient for the pre/post-modification stiffnesses was 0.99 (Figure 4). The common reasons for ROI modifications are summarized in Figure 5. Eighty-three exams were noted as having processing errors. Of these, 43 were not liver MRE and were unintentionally pushed to ALEC. The other 40 cases failed due incomplete or wrong series being sent to ALEC. Once the correct images were sent, the processing was done successfully. Processing errors did not prevent subsequent cases from running. Technicians reported that the fully manual workflow, currently only used as a backup option, takes 15-20 minutes per case while the ALEC workflow took 5-10 minutes on average.Discussion
The new semiautomated workflow performed well in the clinical practice. To our knowledge, it did not fail to process any exams for which the complete set of correct images was transferred. Fewer than 3% of the automatic ROIs were modified to remove appreciable nonliver tissue (categories A and B in Figure 5). Over 80% of the automatic ROIs were accepted without any modification by the experienced readers, while the modifications in the other exams resulted in a stiffness difference that was much smaller than typical intra- and inter-reader variabilities of 10% for experienced readers.2-5 Thus, the semiautomated workflow is likely to significantly improve the reproducibility of the liver stiffness measurement.
Automated ROIs that were modified by readers to substantially increase ROI area, without noticeably affecting the stiffness (category C), mostly occurred in images with high vessel contrast (e.g. acquired after contrast injection). Cases where the modified stiffness differed by >10% resulted from inclusion of vessels which reduced apparent stiffness on the elastogram, or low-contrast non-liver tissue with different stiffness (tumors, kidney, gallbladder). ROI modifications which did not lead to a change in stiffness or visible exclusion of nonliver tissue (Category D) were in regions with small to moderate blood vessels or little to moderate wave interference, the exclusion of which is subjective and varies between readers.
Conclusions
The semiautomated ALEC workflow has replaced manual MRE analysis at our institution and has operated successfully for over 2 years. It has a low failure rate, requires relatively infrequent, often small, modifications to the ROIs and is likely to substantially reduce inter/intra-reader variability. ALEC speeds up processing, and allows batch processing of large datasets using a standardized method.Future Work
1) Develop a platform which will allow ALEC to be used at many institutions.
2) Improve the sensitivity and specificity for excluding vessels which affect the elastogram.
3) Adapt ALEC to work with MRE data from other vendors.
Acknowledgements
This work was supported by NIH EB07593, NIH EB001981References
(1) Muthupillai R; Lomas, DJ; Rossman, PJ; Greenleaf, JF; Manduca, A; Ehman, RL. "Magnetic resonance elastography by direct visualization of propagating acoustic strain waves". Science. 1995 Sep 29;269(5232):1854-7.
(2) Dzyubak B, Venkatesh SK, Manduca A, Glaser K, Ehman RL. Automated Liver Elasticity Calculation for MR Elastography. Magn Reson Imaging. 2016 May;43(5):1055-63.
(3) Singh S, Venkatesh SK, Wang Z, Miller FH, Motosugi U, Low RN, Hassanein T, Asbach P, Godfrey EM, Yin M, Chen J, Keaveny AP, Bridges M, Bohte A, Murad MH, Lomas DJ, Talwalkar JA, Ehman RL. Diagnostic performance of magnetic resonance elastography in staging liver fibrosis: a systematic review and meta-analysis of individual participant data. Clin Gastroenterol Hepatol. 2015 Mar;13(3):440-451.e6.
(4) Serai SD, Obuchowski NA, Venkatesh SK, Sirlin CB, Miller FH, Ashton E, Cole PE, Ehman RL. "Repeatability of MR Elastography of Liver: A Meta-Analysis." Radiology. 2017 Oct;285(1):92-100
(5) Zhang J, Arena C, Pednekar A, Lambert B, Dees D, Lee VV, Muthupillai R. Short-Term Repeatability of Magnetic Resonance Elastography at 3.0T: Effects of Motion-Encoding Gradient Direction, Slice Position, and Meal Ingestion. J Magn Reson Imaging. 2016 Mar;43(3):704-12
Figures