5562
Impact of Carotid Endarterectomy on Functional Connectivity1University of Arizona, Tucson, AZ, United States, 2Biomedical Engineering, University of Arizona, Tucson, AZ, United States, 3NICHD, National Institutes of Health, Rockville, MD, United States, 4Medical Imaging, University of Arizona, Tucson, AZ, United States, 5Siemens Healthcare, Tucson, AZ, United States, 6Psychology, University of Arizona, Tucson, AZ, United States, 7Surgery, University of Arizona, Tucson, AZ, United States
Synopsis
Carotid endarterectomy (CEA) as a procedure has been shown effective in reducing the risk of stroke for patients with severe stenosis. The impact of CEA on the functional connectivity of the brain has not been assessed to this point. Nine patients underwent resting state fMRI pre-operatively and 1 month and 6 months post-operatively. Analysis was performed using seed based analysis and matrix based analysis to determine if there were functional connectivity changes as a result of CEA. Seed based and matrix based analysis showed that there were significant functional connectivity changes as result of CEA.
Introduction
Carotid artery stenosis secondary to atherosclerotic disease is associated with increased risk of stroke, but it is not clear if carotid stenosis has long-term cognitive impact (1). Carotid endarterectomy (CEA), surgery to remove carotid plaque, decreases stroke risk, but whether CEA affects brain function and long-term cognition is unknown. To address this issue, the current study was carried out to determine the impact of CEA on the functional connectivity in the brain as assessed via resting state functional MRI and neurocognitive evaluation. We expect this study to help identify quantifiable measures to evaluate neurocognitive function in this population as well as evaluate the contribution of vascular disease to cognitive dysfunction.Methods
Nine patients (6 male/3 female, age 70 ± 6.6 years) with asymptomatic >70% internal carotid artery stenosis (6 left side and 3 right side) who were scheduled to undergo CEA, were enrolled in this study. Patients underwent standardized cognitive testing using the Montreal Cognitive Assessment (MoCA) preoperatively and at 4-6 months post-operatively. In addition, patients underwent resting state fMRI prior to CEA, and 1 month and 4-6 months after CEA on a 3T scanner (Siemens, Skyra). Structural T1 weighted images using an MPRAGE sequence were also acquired for registration. EPI images for rs-fMRI were acquired with a TR/TE=1200/30 msec, FOV=270 mm x 270 mm x 135 mm, FA= 62, acquisition matrix=90x90x45, slice thickness=3 mm, and multi-band factor=3. Data was preprocessed using SPM, FSL and Matlab. Motion and field map correction was performed using SPM. Images were then processed through FSL with registration to MNI (Montreal Neurological Institute) standard space. Independent component analysis was performed to ensure data quality and consistency. Further analysis was performed through seed based analysis and network analysis through correlation matrices. For each subject, a seed was placed in the posterior cingulate cortex to examine the functional connectivity using the FEAT toolbox in FSL. The PCC was selected as an initial seed point due to its involvement in the default mode network and high connection to neurocognitive diseases (2). Correlation matrices were obtained for each subject based on the AAL atlas, which includes 116 regions of interest. To obtain the correlation matrices a mean time series was calculated using all of the voxels within each region. Pearson’s correlation coefficients were calculated for each pair of brain regions and results were combined into a 116x116 matrix. The correlation matrices for the different time points were compared using repeated measures analysis of variance (RM-ANOVA). Post-hoc analyses were performed for all pairs (Baseline-1Month, Baseline-6Month, and 1Month-6Month) for any data that showed significant functional connections to determine when the differences occurred.Results
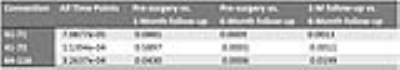
Group mean correlation maps, from points seeded in the PCC, at the three different time points are shown in Figure 1. Visual differences can be seen in regions corresponding to the default mode network. A higher-level analysis that compared pre-operative to both post-operative time points are shown in Figure 2 and exhibit clusters of statistically significant differences with, pre-operative > post-operative in Brodmann Area (BA)11 and in the left hemisphere at BA39 and BA7. In the post-operative > pre-operative clusters of differences are seen in the right hemisphere at BA23 and BA39 and the left hemisphere at BA19. These regions are associated with decision-making, visuomotor coordination, visual comprehension, language, attention and memory. Correlation matrices of a representative subject are shown in Figure 3. Analysis of matrices of all subjects using RM-ANOVA with Bonferroni correction showed a significant difference in the three-time points between the bilateral caudate nucleus (AAL-IDs 71 and 72) and left amygdala (AAL-ID 41) and between the right supramarginal area (AAL-ID 64) and Vermis 10 (AAL-ID 116). The p-values for post-hoc analysis comparing each pair of time points are shown in Table 1. Significant changes (p<0.05) occurred when comparing 6-month results to other time points, as well as baseline to 1 month for AAL-ID 64-AAL-ID 116. In addition to MRI-detected differences, MoCA scores showed significant improvement 4-6 months after CEA compared to pre-operative testing (p<0.05), as shown in Figure 4.Discussion
Significant changes in functional connectivity were observed in all patients who underwent CEA. Analysis performed with a PCC seed point showed significant changes in regions that are associated with executive function and memory. Matrix analysis demonstrated differences in connectivity between regions associated with storing and processing of memory. These observed changes from rs-fMRI are associated with an overall improved performance on a neurocognitive assessment (MoCA). Comparisons between additional neurocognitive test results and structural connectivity will guide further study into which regions of the brain may benefit from CEA.Acknowledgements
This work was supported by the Arizona Health Sciences Center Translational Imaging Program Project Stimulus (TIPPS) FundReferences
1. Inzitari D, Eliasziw M, Gates P, Sharpe BL, Chan RKT, Meldrum HE, Barnett HJM. The Causes and Risk of Stroke in Patients with Asymptomatic Internal-Carotid-Artery Stenosis. N. Engl. J. Med. 2000;342:1693–1701. doi: 10.1056/NEJM200006083422302.
2. Leech R, Sharp DJ. The role of the posterior cingulate cortex in cognition and disease. Brain 2014;137:12–32. doi: 10.1093/brain/awt162.
Figures