5556
Resting-State Fractional ALFF and Seed-Based Analysis as a Function of Bladder Discomfort1Biomedical Engineering, Stony Brook University, Stony Brook, NY, United States, 2Urology, Stony Brook University, Stony Brook, NY, United States, 3Radiology, Stony Brook University, Stony Brook, NY, United States
Synopsis
The neural mechanisms underlying over active bladder are not fully understood. In addition, the neural network involved in bladder control hasn’t been identified. In this study, we looked at resting-state functional MRI of healthy females as a function of bladder filling, utilizing fractional amplitude of low frequency fluctuation (fALFF) and seed-based functional connectivity measures. Our results demonstrate modulated activation amplitude and functional connectivity throughout the brain, primarily characterized by increases in the anterior brain, furthering our understanding of bladder control and setting the foundation for additional higher level analyses.
Introduction
Over active bladder (OAB) is characterized by the frequent desire to urinate that cannot be suppressed. This disorder affects ~15% of women in the US and most treatment options are ineffective. Currently, knowledge of the mechanisms underlying OAB in women is limited with no clear link to anatomical abnormalities. Studies have identified functional abnormalities in a similar disorder, irritable bowel syndrome, leading to the hypothesis that OAB has neurological foundations1. In this study, bladder filling induced changes in resting-state activation and functional connectivity patterns in healthy females were measured. By identifying activation and rs-fcMRI patterns during bladder filling, we can obtain a more comprehensive understanding of the brain’s response to filling.Methods
Nine healthy female participants were studied. Resting-state BOLD fMRI (3.5x3.5x5.0mm3, TR=4s, 116 time points per session) and T1-weighted MRI (1x1x1mm) were acquired on a Siemens 3T Prisma MRI. Subjects voided their bladder prior to imaging. Direct catheterization was used to fill the bladder with water in step-wise intervals of 0, 50, 100, 200, 350, and 500mL. Urgency levels were self-reported at each interval. Bladder filling and imaging had to be stopped after 350mL for 2 subjects.
Data analyses were carried out in MATLAB with CONN (www.nitrc.org/projects/conn) and SPM12 (www.fil.ion.ucl.ac.uk/spm) toolboxes. Preprocessing of fMRI data included within-subject realignment, temporal smoothing, outlier volume detection (peak-to-peak motion threshold=0.5mm, global signal z-value threshold=3), normalization to MNI space after coregistration with T1w image, spatial smoothing with a 5mm FWHM Gaussian kernel, nuisance and motion regression using aCompCor2 and motion scrubbing, and bandpass filtering between 0.01-0.1Hz. Whole-brain fractional amplitude of low frequency fluctuation (fALFF3) analysis was performed, allowing us to probe the relative voxel-wise strength of low frequency oscillations (LFO, 0.01-0.1Hz). Seed-to-voxel whole-brain analysis was carried out using 8 seed regions based on fALFF results: L/R Middle Temporal Gyrus (MTG), L/R Middle Frontal Gyrus (Frontal Pole, FP), L/R Insular Cortex (IC) and L/R Superior Temporal Pole (TP) derived from the 90-parcellation AAL atlas4.
Statistical tests for bladder filling differences in fALFF and functional connectivity were carried out via the general linear model (GLM), utilizing t-tests. Data from 0mL and 50mL filling, and from 350mL and 500mL filling, were averaged to create low and high urgency states for comparison. Voxel-wise significance was set at a threshold of p<0.005 (uncorrected), while false discovery rate correction was performed on cluster size statistics with a threshold of p-FDR<0.05.
Results
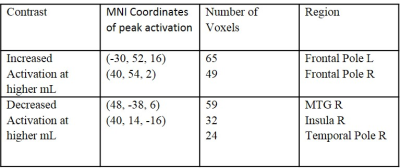
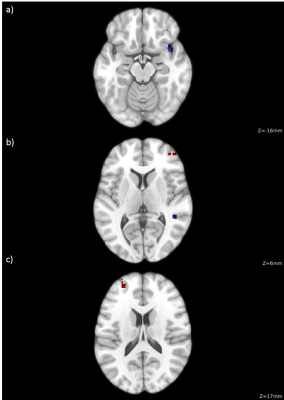
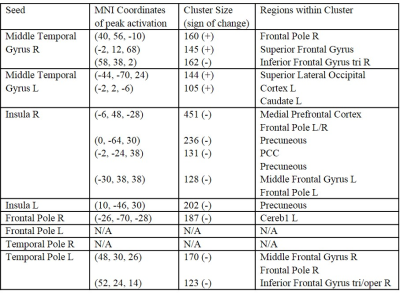
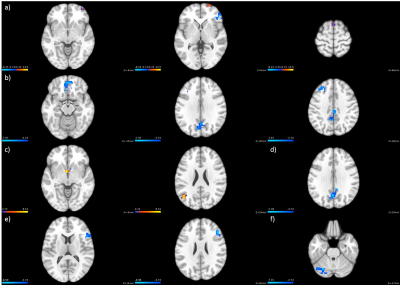
fALFF analysis revealed significantly higher LFO amplitude in the bilateral FP, and significantly lower LFO amplitude in the right IC, right MTG and right TP with respect to bladder fullness (Table 1, Figure 1). Seed-based analysis revealed significant connectivity changes in the bilateral MTG, bilateral IC, right FP and left TP (Figure 2). Results are summarized in Table 2.
Altered connectivity with clusters in the bilateral FP was observed in the bilateral IC and left TP. A clear decrease in IC connectivity with large clusters in resting-state hubs (mPFC, PCC/Precuneous) was also observed. Higher connectivity to the SFG and the right FP was observed in the right MTG. Lower connectivity was observed in similar regions (MidFG, right FP) in the left TP. Both seeds also showed decreased connectivity to a cluster in the pars triangularis.
Discussion
This study observed several fMRI-related changes associated with bladder filling. Heightened relative activation amplitude in the FP is likely indicative of increased effort to control muscles as urgency to urinate increases. Significant changes to IC connectivity and activation are consistent with existing literature on OAB patients, which found increased perfusion and activation as a function of urgency5. Decreased connectivity to default mode regions suggests IC connectivity modularity as the subjects became more engaged in controlling their urge. Similarly, decreased MTG activation amplitude and increased bilateral MTG connectivity to control and motor related regions (SFG, Caudate, etc.) could be indicative of modularity.
When probing results that barely failed to reach statistical significance, we noticed a widespread pattern in increased frontal activation amplitude and decreased medial-posterior activation amplitude. Further probing of these regions with a larger sample size and higher level analyses, such as graph theory, may reveal the underlying mechanisms of bladder control.
Conclusion
This study demonstrated differences in BOLD rs-fMRI neural networks at high and low urgency states under bladder filling. This cohort displayed a clear pattern of widespread increased relative frontal activation strength along with decreases in medial-posterior regions, as well as functional connectivity changes indicative of modularity correlated with urgency and bladder control. This study lays the foundation for studying patients with OAB, which could provide insight into the neurological mechanisms involved in OAB disorder.Acknowledgements
No acknowledgement found.References
1. Yuan Y-Z, Tao R-J, Xu B, et al. Functional brain imaging in irritable bowel syndrome with rectal balloon-distention by using fMRI. World Journal of Gastroenterology : WJG. 2003;9(6):1356-1360. doi:10.3748/wjg.v9.i6.1356.
2. Behzadi Y, Restom K, Liau J, Liu TT. A Component Based Noise Correction Method (CompCor) for BOLD and Perfusion Based fMRI. NeuroImage. 2007;37(1):90-101. doi:10.1016/j.neuroimage.2007.04.042.
3. Zou Q-H, Zhu C-Z, Yang Y, et al. An improved approach to detection of amplitude of low-frequency fluctuation (ALFF) for resting-state fMRI: Fractional ALFF. Journal of neuroscience methods. 2008;172(1):137-141. doi:10.1016/j.jneumeth.2008.04.012.
4. N. Tzourio-Mazoyer, B. Landeau, D. Papathanassiou, F. Crivello, O. Etard, N. Delcroix, B. Mazoyer, M. Joliot. Automated Anatomical Labeling of Activations in SPM Using a Macroscopic Anatomical Parcellation of the MNI MRI Single-Subject Brain. NeuroImage. 2002:15(1):273-289. https://doi.org/10.1006/nimg.2001.0978.
5. Arya NG, Weissbart SJ, Xu S, Bhavsar R, Rao H. Quantitative Changes in Cerebral Perfusion during Urinary Urgency in Women with Overactive Bladder. BioMed Research International. 2017;2017:2759035. doi:10.1155/2017/2759035.
Figures