5506
Investigation of tumor bed effect of radiotherapy using vessel size imaging in animal prostate cancer1Dept. Medical Imaging and Intervention, Chang Gung Memorial Hospital, Linkou, Taiwan, 2Dept. Medical Imaging and Radiological Sciences, Chang Gung University, Taoyuan, Taiwan, 3Dept. Radiation Oncology, Chang Gung Memorial Hospital, Linkou, Taiwan
Synopsis
MR-derived estimates of vessel size and vascular density were used to investigate the microvasculature change of tumor following preirradiation on tumor bed. The hypoxic area exhibited higher vessel size and reduced microvascular density compared with those in normoxic area. The alterations of the derived estimates were more pronounced in hypoxic regions. Significantly positive correlations were found between MRI and histology measurements. The vessel size imaging technique may be used as an imaging biomarker to characterize the tumor bed effect that occurs in recurrent tumor after radiotherapy.
INTRODUCTION
Patients with recurrent local tumor after radiotherapy have increased probability of developing metastases. Tumor transplants in preirradiated (pre-IR) tissues have shown greater metastatic propensity than in nonirradiated tissues, a phenomenon known as the tumor bed effect (TBE). An inadequate vasculacture from the pre-IR tissue is considered to be responsible for TBE 1. This study aims to investigate if the MR-derived vessel size imaging (VSI) can be used to as an imaging biomarker for TBE in pre-IR prostate tumor model.
METHODS
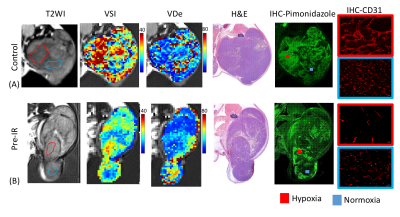
Tumors were generated by inoculation of transgenic adenocarcinoma of the mouse prostate (TRAMP)-C1 cancer cells into the thigh. MRI experiments were performed at 6, 10,14 and 20 days following tumor inoculation using a 7-Tesla animal MR scanner. The pre-IR group (n=6) received a single dose of 25 Gy immediately before tumor implantation. The control group (n=6) received no irradiation. The MRI protocol included T1 weighted imaging, T2 weighted imaging and diffusion weighted imaging. VSI was performed using a multi gradient echo and a multi spin echo sequences, which were acquired prior to and 4 minutes after administration of ultrasmall superparamagnetic iron oxide (USPIO) (P904, Guerbet, France)2,3. The relaxation rates of ∆R2 and ∆R2* were obtained to calculate the vessel density estimate as: VDe = 329 (∆R2)3/(∆R2*)2 . The vessel size index was calculated as: VSI=0.424(ADC/γ∆χB0)1/2 (ΔR2*/ΔR2)3/2 , where ADC was the diffusion coefficient of the corresponding pixel, γ and B0 represent gyromagnetic ratio and stationary field, respectively. ∆χ was considered equal to 0.57 ppm4.
Histology: The orientation of MRI and histology were matched using a pre-embedding technique 5. Tumor sections were stained by hematoxylin and eosin (H&E), pimonidazole in detecting hypoxia and CD31 as a marker for endothelial cells. Vessel size was determined by the average of diameters of long and short axes of vessels in the field. Microvascular density was determined as the number of vessels in the field.
RESULTS
In both the Pre-IR and control groups, the hypoxic area exhibited significantly higher vessel size and reduced microvascular density compared with those in normoxic area (P < .001). The pre-IR group showed increased vessel size and reduced vascular density in hypoxic regions compared with those in control group (P < .01 for both MRI and histological estimates). In normoxic area, VDe was slightly lower in Pre-IR group compared with that in control group (P = .041). No significant difference was found in MRI- and histology-derived vessel size indices in normoxic areas (P > 0.05). Significantly positive correlations were found between MRI and histology measurements in both the vessel size and density estimates in hypoxic areas (P < .01).DISCUSSION
Our results indicate that MRI mapping of the vessel size and density is sensitive to the change of microvasculature in pre-IR prostate tumor. The observed vessel dilation in hypoxic tumor may be attributed to increased local demand for oxygen because of a change in metabolic activity in the tumor. The decreased vascular density and relatively smaller vessel size in pre-IR tumor may be associated with diffusion limited chronic hypoxic caused by vascular deficiency.CONCLUSION
The vessel size imaging technique may be used as an imaging biomarker to characterize the tumor bed effect that occurs in recurrent tumor after radiotherapy.Acknowledgements
Supported by Chang Gung Medical Foundation grant CIRPG3D0161-3,, Ministry of Science and Technology, R.O.C MOST 105-2314-B-182A-066, MOST 106-2314-B-182A-016 -MY2.References
1. Chen FH, Chiang CS, Wang CC, et al. Vasculatures in tumors growing from preirradiated tissues: formed by vasculogenesis and resistant to radiation and antiangiogenic therapy. Int J Radiat Oncol Biol Phys. 2011;80(5):1512-1521.
2. Lemasson B, Valable S, Farion R, Krainik A, Remy C, Barbier EL. In vivo imaging of vessel diameter, size, and density: a comparative study between MRI and histology. Magn Reson Med. 2013;69(1):18-26.
3. Tropres I, Pannetier N, Grand S, et al. Imaging the microvessel caliber and density: Principles and applications of microvascular MRI. Magn Reson Med. 2014.
4. Tropres I, Lamalle L, Peoc'h M, et al. In vivo assessment of tumoral angiogenesis. Magn Reson Med. 2004;51(3):533-541.
5. Lin YC, Wang CC, Lin G, et al. A simple method to improve the quality of diffusion-weighted magnetic resonance imaging with rapid histologic correlation in a murine model. Molecular imaging. 2014;13(0):1-8.
Figures