5427
White Matter Integrity in Adolescents with Attention Deficit Hyperactivity Disorder with Comorbid Bipolar Disorder assessed by Tract Based Spatial Statistics1National Magnetic Resonance Research Center (UMRAM), Bilkent University, Ankara, Turkey, 2Department of Child and Adolescents Psychiatry, On Dokuz Mayis University, Samsun, Turkey, 3Department of Radiology, On Dokuz Mayis University, Samsun, Turkey, 4Department of Child and Adolescents Psychiatry, Kocaeli University, Kocaeli, Turkey, 5Department of Child and Adolescents Psychiatry, Hacettepe University, Ankara, Turkey, 6Department of Radiology, Hacettepe University, Ankara, Turkey, 7Department of Radiology, Kocaeli University, Kocaeli, Turkey
Synopsis
White matter (WM) integrity is an important factor for the pathophysiology of attention-deficit/hyperactivity disorder (ADHD) and bipolar disorder (BD) in adolescents. In this study, we hypothesized that adolescents with attention deficit hyperactivity disorder with comorbid bipolar disorder (ADHD+BD) would yield different pattern and extent of WM abnormalities than ADHD and BD. Sixty adolescents were categorized into four groups as ADHD, BD, ADHD+BD and healthy controls. The comparative diffusion tensor imaging analyses were performed between each patient group and healthy controls. Adolescents with ADHD+BD displayed different pattern and extent of WM abnormalities than ADHD and BD revealed by tract-based spatial statistics.
Purpose
Recent studies have shown that white matter (WM) abnormalities have important roles in the pathophysiology of attention-deficit/hyperactivity disorder (ADHD) and bipolar disorder (BD) in adolescents1, 2. We hypothesized that adolescents with attention deficit hyperactivity disorder with comorbid bipolar disorder (ADHD+BD) would yield different pattern and extent of WM abnormalities than ADHD and BD adolescents revealed by tract based spatial statistics (TBSS).Methods
Subjects: Sixty age-, sex- and handedness-matched adolescents (ADHD: n=15, BD: n=15, ADHD+BD: n=15, healthy controls: n=15, age range: 12–18 years) were included in the study. All adolescents were diagnosed on the basis of clinical findings and their parents were also matched with age, socio-economic and education status (p>0.05).
Image Acquisition: Imaging protocol included isotropic high resolution diffusion tensor imaging (DTI) of the whole brain (single-shot EPI; TR/TE: 4332/101 ms, max. b factor: 800 s/mm2, 32 independent directions, FOV: 224 mm, matrix: 128×128, voxel size: 2x2x2 mm, 60 axial sections with 2 mm thickness, no intersection gap). All experiments were performed on a 3T MR scanner (Philips, Ingenia, Netherlands).
Data Processing and Analysis: The comparative DTI analyses of the groups were performed using tract-based spatial statistics (TBSS), a part of FSL software3. Head motion and eddy-current correction, skull stripping and diffusion tensor fitting (FSL DTIFit) steps were performed for the preprocessing of the diffusion-weighted data. Then fractional anisotropy (FA) maps were computed. Registration and alignment of FA maps to the average space and computation of the thinned mean FA skeleton were performed. To perform voxelwise statistics, the permutation-based inference with 500 permutations were used. The resulting threshold-free cluster enhancement output was corrected for multiple comparisons by controlling the family-wise error rate and thresholded at significance level p < 0.05. The standard cluster-based thresholding was applied with a t threshold of 1.5 for the multiple comparisons. The contiguous clusters of supra-threshold voxels were obtained using 26-neighbour connectivity. Total number of significant voxels in each group comparison were calculated.
Results
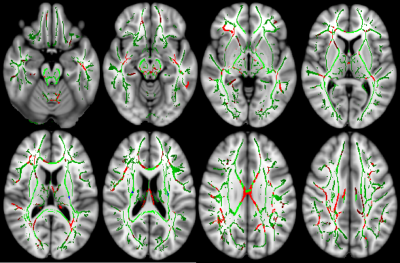
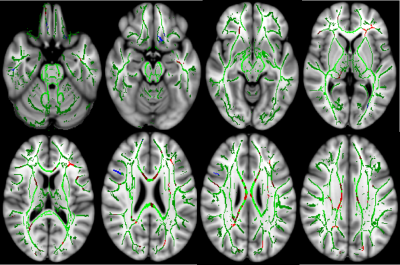
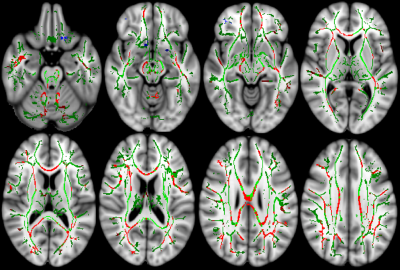
Adolescents with BD showed significantly reduced FA in bilateral cerebral peduncle (CP), cingulum, and fornix, right anterior limb of internal capsules (ALIC), genu and body of corpus callosum (CC) and right superior longitudinal fasciculus (SLF) compared with healthy controls (Fig. 1) (p<0.05). Adolescents with ADHD showed FA reduction in right ALIC, body and genu of CC and bilateral corticospinal tracts compared to healthy controls (Fig. 2) (p<0.05). When compared to healthy controls, TBSS results revealed that adolescents with ADHD+BD showed significant FA reduction in bilateral CP, cingulum, external capsules, posterior and superior corona radiata, right hippocampus, and body, genu and splenium of CC (Fig. 3) (p<0.05). Widespread FA reduction in ADHD+BD was also seen as a result of total number of significant voxels: BD (19032), ADHD (6534), ADHD+BD (27513). There was no significant change in FA elevation between the groups.Discussion and Conclusion
TBSS analysis of DTI data revealed that adolescents with attention deficit hyperactivity disorder with comorbid bipolar disorder displayed different pattern and extent of white matter abnormalities. The results may also reveal important insights into the long term prognosis of attention-deficit/hyperactivity disorder, etiology of both attention-deficit/hyperactivity disorder and bipolar disorder and comorbidity of bipolar disorder.Acknowledgements
This project founded by On Dokuz Mayis University Research Project Management System (Project Number: PYO.TIP.1902.15.004).References
1. Pavuluri MN, Yang S, Kamineni K, et al. Diffusion Tensor Imaging Study of White Matter Fiber Tracts in Pediatric Bipolar Disorder and Attention-Deficit/Hyperactivity Disorder. Biol Psychiatry. 2009;65(7):586-593.
2. Tamm L, Barnea-Goraly N, Reiss AL. Diffusion tensor imaging reveals white matter abnormalities in Attention-Deficit/Hyperactivity Disorder. Psychiatry Res. 2012;202(2):150-154.
3. Jenkinson M, Beckmann CF, Behrens TE, et al. Fsl. Neuroimage. 2012;62(2):782-90.
Figures