5403
Low Apparent Diffusion Coefficient Value Predicts Early Progression of Skull Base Meningiomas1Medical Imaging, Chi Mei Medical Center, Tainan, Taiwan, 2Neurosurgery, Chi Mei Medical Center, Chiali, Tainan, Taiwan, 3Radiology, E-Da Hospital/I-Shou University, Kaohsiung, Taiwan, 4Center for Functional Onco-Imaging, University of California Irvine, Irvine, CA, United States, 5Pathology, Chi Mei Medical Center, Tainan, Taiwan, 6Institute of Biomedical Science, National Sun Yat-Sen University, Kaohsiung, Taiwan
Synopsis
A recent study described the extent of tumor resection and ADC values could offer better prediction of progression/recurrence (P/R) in meningiomas than histopathological grading. Although complete resection of tumor is a key determining factor of recurrence in meningiomas, it is often difficulty to achieve for the skull base meningiomas (SBM) due to complex neurovascular structures. In this study, we investigated the preoperative CT and MR imaging features for the prediction of early P/R in SBM, with emphasis on ADC values. Our results found that low ADC value and adjacent bone invasion could predict high risk of early P/R in SBM, and therefore, offer clinically vital information for the planning of treatment.
Background and Purpose:
Meningiomas constitute about 33.8% of all primary brain tumors, and 20 to 30% of these meningiomas are found in the skull base (1, 2). Although meningiomas are classified into WHO grade I (benign), grade II (atypical), and grade III (anaplastic/malignant) based on the 2007 WHO classification system, a subset of WHO grade I meningiomas show early progression/recurrence (P/R) in the first years after surgical resection (3-6). Several studies have reported high diffusion-weight imaging (DWI) and lower apparent diffusion coefficient (ADC) values (more restricted diffusion) are related to atypical or malignant meningiomas (7, 8); however, the correlation of ADC values and clinical outcomes has rarely been mentioned. A recent study described the extent of surgical resection and ADC values could offer better prediction of P/R in meningiomas than histopathological grading (9). However, complete surgical resection, recognized as Simpson Grade I resection, is often difficulty to achieve for the skull base meningiomas (SBM) due to complex neurovascular structures (2, 10). On the other hand, most SBM are WHO grade I benign tumors, and conservative follow up or subtotal tumor resection to avoid subsequent surgical complications are treatment choices in complicated cases (11). Therefore, the one main challenge in the treatment of SBM is to determine factors that correlate with early P/R. Additionally, the role of adjuvant radiotherapy (RT) for low-grade meningiomas is unclear, therefore, practice varies greatly among institutions. In this study, we will investigate the preoperative CT and MR imaging features for the prediction of early P/R in SBM, with emphasis on ADC values. The benefit of adjuvant RT for prevention of early P/R in SBM will also be investigated.
Materials and Methods:
This retrospective included patients with pretreatment brain CT and MRI including DWI and corresponding ADC imaging, and were sequentially diagnosed with SBM (WHO grade I, II, and III) by pathological confirmation. Only patients with postoperative MRI follow-ups for more than 1 year (at least every 3-6 months) were included according to previous references (6, 9). Preoperative brain CT was performed routinely for navigation (stereotactic surgery) in our hospital. From October 2006 to December 2015, total 78 patients (20 men, 58 women, age 26-85 years) were included. The median follow-up time was 40 months (ranging from 12 to 115 months). In 19 patients with early P/R, the median time to P/R was 27 months (ranging from 2 to 56 months). The MRI images were acquired using a 1.5T (Siemens, MAGNETOM Avanto) (N = 31), a 1.5T (GE Healthcare, Signa HDxt) (N = 32), or a 3T (GE Healthcare, Discovery MR750) (N = 15) MR scanners, equipped with 8-channel head coils. The protocols of MR imaging were as the following: axial and sagittal spin-echo T1WI, fast spin-echo T2WI, fluid attenuated inversion recovery (FLAIR), T2*-weighted gradient-recalled echo (GRE). Contrast-enhanced images were obtained in axial and coronal T1WI. The DWI was performed by applying sequentially in the x, y, and z direction with b =1000 sec/mm2 or 1500 sec/mm2, and ADC maps were obtained from these imaging data. For ADC measurement, a circular ROI (area ranging from 32 to 75 mm2) was placed within the tumor area. For normalization of individual variance, ADC ratio was calculated by dividing the ADC value of the tumor by the ADC value of contralateral normal-appearing cerebral white matter (NAWM) in the same patient. Statistical analyses were performed to assess preoperative qualitative CT/MRI imaging features and quantitative ADC values/ratios between SBM with and without early P/R. Thirty-four patients received postoperative adjuvant RT.
Results:
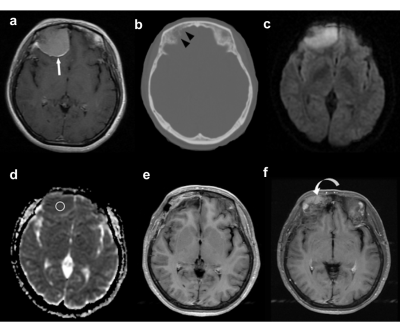
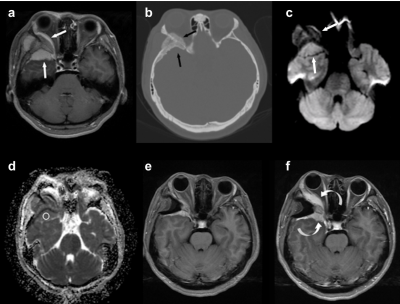
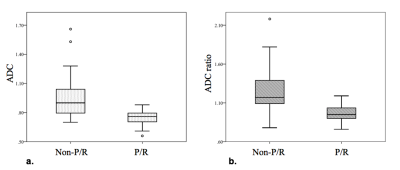
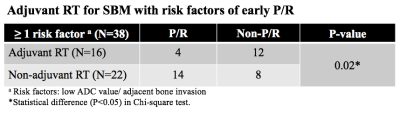
Nineteen (19/78, 24.3%) patients had early P/R. Most of the SBM (73/78, 93.6%) were WHO grade I tumor. No statistical significant differences in extent of tumor resection (P=0.69) and postoperative adjuvant RT (P=0.08) between patients with (N=19) and without (N=59) early P/R. SBM with spheno-orbital location, adjacent bone invasion, high DWI, and lower ADC value/ratio were significantly associated with early P/R (P<0.05) (Figures 1-3). The cut-off points of ADC value and ADC ratio for prediction of early P/R are 0.83 x 10-3 mm2/s and 1.09 respectively, with excellent sensitivity and AUC (P<0.05). In multivariate logistic regression analysis, low ADC value (< 0.83 x 10-3 mm2/s) and adjacent bone invasion predict high risk of early P/R with odds ratios of 47.73 and 17.56 respectively. For patients (N=38) with high risk factors of early P/R, adjuvant RT provided significant benefit in preventive measures (P<0.05) (Figure 4).
Conclusions:
Low ADC value and adjacent bone invasion predict high risk of early P/R in SBM, and therefore, offer clinically vital information for the planning of treatment. Furthermore, for patients with high risk factors of early P/R, adjuvant RT offers significant benefit in preventive measures.Acknowledgements
NoneReferences
1. Wiemels J. Journal of neuro-oncology. 2010;99(3):307-14.
2. Mansouri A. Journal of neurosurgery. 2016;125(2):431-40.
3. Louis DN. Acta neuropathologica. 2007;114(2):97-109.
4. Perry A. The American journal of surgical pathology. 1997;21(12):1455-65.
5. Maillo A. Neuro-oncology. 2007;9(4):438-46.
6. Ildan F. Skull base: official journal of North American Skull Base Society [et al]. 2007;17(3):157-71.
7. Nagar VA. American journal of neuroradiology. 2008;29(6):1147-52.
8. Tang Y. American journal of roentgenology. 2014;202(6):1303-8.
9. Hwang WL. Neuro-oncology. 2016;18(6):863-72.
10. Nanda A. Skull base: official journal of North American Skull Base Society [et al]. 2008;18(4):243-52.
11. Sekhar LN. Neurosurgery. 2015;62 Suppl 1:30-49.
Figures