5369
Brain axonal and myelin changes after positive airway pressure treatment in patients with obstructive sleep apneaAshish Kaul Sahib1, Bhaswati Roy2, Xiaopeng Song1, Sadhana Singh1, Luke Ehlert1, Ravi Aysola3, Daniel Kang3, Mary Woo2, and Rajesh Kumar1,4,5,6
1Departments of Anesthesiology, University of California at Los Angeles, Los Angeles, CA, United States, 2UCLA School of Nursing, University of California at Los Angeles, Los Angeles, CA, United States, 3Medicine, University of California at Los Angeles, Los Angeles, CA, United States, 4Radiological Sciences, University of California at Los Angeles, Los Angeles, CA, United States, 5Brain Research Institute, University of California at Los Angeles, Los Angeles, CA, United States, 6Bioengineering, University of California at Los Angeles, Los Angeles, CA, United States
Synopsis
Newly-diagnosed, treatment-naïve obstructive sleep apnea subjects show predominately acute tissue changes in gray and white matter, in addition to autonomic, mood, and cognitive deficits, but the extent of brain tissue recovery after PAP treatment and required minimum treatment time is unclear. We examined brain axonal and myelin changes at baseline and tissue recovery after 3 and 9 months’ positive airway pressure treatment in OSA compared to control subjects. Our findings indicate that brain structural changes found in newly-diagnosed OSA subjects can be reversible with long-term PAP treatment.
Introduction
Obstructive sleep apnea (OSA), a condition characterized by persistent events of partial or complete upper airway obstruction, with continued diaphragmatic efforts to breathe during sleep, results in significant brain damage, in addition to autonomic, mood, and cognitive deficits. The predominant brain tissue changes are in acute stage in newly-diagnosed, treatment-naive OSA subjects and appear in white matter (WM) axons and myelin (1), in addition to gray matter, in sites that are involved in serving multiple functions, including autonomic, mood and cognitive functions (1, 2). Since majority of tissue changes are in acute stage, such deficits may be resolved/recovered by positive airway pressure (PAP; forced air through the airway to maintain potency). However, the extent of brain tissue recovery after PAP treatment and required minimum treatment time in newly-diagnosed OSA subjects is unclear. Our aim was to examine myelin and axonal changes, derived from diffusion tensor imaging (DTI) indices, in newly-diagnosed, treatment-naive OSA subjects after 3 and 9 months adequate use of PAP. We hypothesized that newly-diagnosed OSA subjects would show axonal and myelin tissue recovery after PAP treatment, and more recovery will be shown at 9 months than 3 months of PAP use.Methods
Fourteen newly-diagnosed, treatment-naïve OSA subjects (age, 47.9±9.3 years; body-mass-index (BMI), 33.0±5.5 kg/m2; 8 males) and 14 age- and gender-matched controls (age, 45.1±8.9 years; BMI, 27.6±3.7 kg/m2; 8 males) were studied. All OSA subjects had a moderate-to-severe diagnosis (AHI ≥15 events/hour), no history of neurological illness or psychiatric disorders other than OSA condition, and were recruited from the Sleep Disorders Laboratory. All participants gave written informed consent before data acquisition and the study protocol was approved by the Institutional Review Board. Control subjects were healthy, without any medications that might alter brain tissue. OSA and control subjects were evaluated at baseline, but OSA subjects were followed at 3-months (14 OSA) and 9-months (9 OSA) after PAP treatment. Brain imaging studies were performed using a 3.0-Tesla MRI scanner (Siemens, Magnetom Prisma). Two separate DTI series were collected using a single-shot echo planar imaging with twice-refocused spin-echo pulse sequence (TR=12,200 ms; TE=87 ms; flip-angle=90°; band width=1,345 Hz/ pixel; matrix size=128×128; FOV=230×230 mm2; slice thickness=1.7 mm, diffusion values=0 and 800 s/mm2, diffusion directions=30). Diffusion (b = 800 s/mm2) and non-diffusion weighted images (b = 0 s/mm2) were used to calculate diffusion tensors, and principal eigenvalues (λ1, λ2, and λ3). These principal eigenvalues were used to calculate AD (λ‖‖ = λ1) and RD [λ⊥ = (λ2 + λ3)/2] values at each voxel. The AD and RD maps, derived from each DTI series, were realigned to remove any potential variation from head motion and averaged. The averaged AD and RD maps were normalized to Montreal Neurological Institute space, smoothed (Gaussian filter, 10 mm), and smoothed maps were compared between OSA and controls using ANCOVA (covariates: age and gender; p<0.005) at baseline, 3-months, and 9-months of PAP treatment.Results
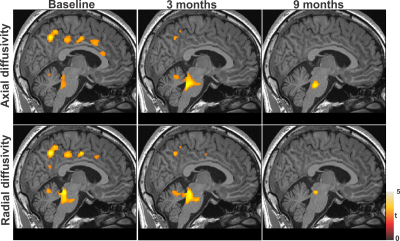
No differences in age (p = 0.43) or gender (p = 0.46) appeared between OSA and control subjects. However, BMI values were significantly higher in OSA vs. controls (p = 0.005). At baseline, OSA subjects showed significantly reduced AD and RD values in multiple areas, including the pons, hippocampus, insula, cingulate and cingulum bundle, cerebellar cortices and white matter, and corona radiate, over control subjects (Fig. 1), suggesting axonal and myelin changes. After 3 months of PAP treatment, few sites with tissue recovery emerged in AD and RD measures in OSA compared to controls (Fig. 1). However, after 9 months of PAP treatment, majority of brain areas showed improvement in AD and RD changes, though deep structures, including midline pons, did not recover completely in OSA compared to controls (Fig. 1).Discussion
Regional brain AD and RD values are significantly reduced in various cardiovascular, mood, and respiratory regulatory sites at baseline in newly-diagnosed OSA over control subjects, indicating predominantly acute axonal and myelin changes injury. The PAP treatment normalizes tissue changes in few sites at 3-months, but most of AD and RD changes in cortical areas and outer regions improve at 9-months, except in deep brain regions. The findings suggest that prolonged PAP usage (> 3 months) is necessary for maximum brain tissue rescue, and thus, associated functional recovery in OSA subjects.Conclusion
This study provides the evidence that structural brain abnormalities observed in newly-diagnosed OSA subjects can be improved with PAP treatment, although long-term treatment is needed for maximum brain structural and functional recovery.Acknowledgements
This work was supported by National Institutes of Health R01 NR-015038 and R01 HL-113251.References
1. Kumar R, Chavez AS, Macey PM, et al. J Neurosci Res. 2012;90:2043-52.
2. Macey PM, Kumar R, Woo MA, et al. Sleep. 2008;31(7):967-77