5316
The morphometric brain alteration in current and remitted major depressive disorder: a meta-analysis1Huaxi MR Research Center (HMRRC), West China Hospital of Sichuan University, Chengdu, China, 2Department of Nuclear Medicine, West China Hospital of Sichuan University, Chengdu, China
Synopsis
To investigate the gray matter volume (GMV) alteration in major depressive disorder (MDD) patients at different episode state, here we conducted a meta-analysis which tried to integrate the Voxel-based morphometry (VBM) studies by using Seed-based d Mapping. This study detected that lower GMV in the left insula in both current and remitted MDD patients compared to HC. And the current conjunction meta-analysis indicated that GMV in bilateral anterior cingulate (ACC) were decreased in current MDD patients but increased in remitted MDD patients. Our findings here motivate a morphological alteration pattern of MDD linked to dynamic mood dysfunction state.
Purpose
Major depressive disorder (MDD) patients has been reported dysfunctions in mood, with widely structure alteration in brain regions relative to health controls (HC) [1][2]. However, it is still not exactly known that the brain abnormalities in comparison of current and remitted MDD patients, which might be lead to the inconsistences of those neuroimaging studies’ results. To investigate the gray matter volume (GMV) alteration in MDD patients at different episode state, here we conducted a meta-analysis which tried to integrate the original studies by using Seed-based d Mapping (http://www.sdmproject.com, SDM).Methods
Results
Finally, this analysis includes 36 datasets recruited 967 MDD patients in current depressed episode and 7 datasets recruited 164 remitted MDD patients (Fig.1). Current MDD patients relative to HC showed decreased GMV in bilateral superior frontal gyrus (SFG), anterior cingulate cortex (ACC) and median cingulate cortex (MCC), left inferior frontal gyrus (LIFG, BA48), and insula, and increased GMV in bilateral cerebellum, hemispheric lobule IV / V and vermic lobule IV / V. Remitted patients had weakly lager GMV in bilateral ACC, right gyrus rectus and left IFG, and lower GMV in left insula IFG, and gyrus rectus compared to HC (Fig. 2). Comparison of effect sizes between current and remitted MDD patients revealed that current MDD patients had lower GM volumes in bilateral ACC, left IFG and right superior temporal gyrus than remitted MDD patents.Discussion
This study demonstrated a distinct pattern of grey matter volumetric change in MDD patients, with converging evidence from meta-analysis comparing current and remitted MDD patients. Importantly, lower GMV in the left insula observed in both current depression and remitted patients compared to HC. A possible explanation to the phenomena is that GMV in the left insula may be influenced by the cognitive-emotion integration pathway, which could not be changed with depressive symptoms recovering at the same time. That is also the reason why MDD patients who have response to cognitive behavioral therapy showed lower levels of functional activity in the insula [4]. Meanwhile, the current conjunction meta-analysis indicated that GMV in bilateral anterior cingulate (ACC) were decreased in current MDD patients but increased in remitted MDD patients. Gray matter reduction in the SFG in MDD patients was reported in previous studies [5], suggesting that SFG is one of the rich hub in brain network contributed to the pathological mechanism in depressive episode. GMV change in bilateral ACC in our finding is consistent with previous research, suggesting that the protective/neurotrophic effects of some antidepressant drugs may restore the decrease in GMV [6]. Only GMV in bilateral cerebellum, hemispheric lobule IV / V and vermic lobule IV / V increased in current MDD patients compared to healthy controls. The pathological mechanism of GMV in cerebellum increased in patients with currently depression episode is not exactly clarified, one possibility may be that cerebellum involved in the “limbic cerebellum networks” which participated in the emotion regulation.Conclusion
Our findings here motivate a morphological alteration pattern of MDD in which grey matter volumetric change is tightly linked to dynamic mood dysfunction state.Acknowledgements
This study was supported by the National Natural Science Foundation (Grant Nos. 81771718, 81621003, 81571637 and 81271532) and Program for Changjiang Scholars and Innovative Research Team in University (IRT16R52) of China. Q.G. would also like to acknowledge the support from his Changjiang Scholar Professorship Award (T2014190) of China and the CMB Distinguished Professorship Award (F510000/G16916411) administered by the Institute of International Education, USA.References
[1]. Wise, T., Radua, J., Via, E., Cardoner, N., & Abe, O. 2016. Common and distinct patterns of grey-matter volume alteration in major depression and bipolar disorder: evidence from voxel-based meta-analysis.
[2]. Anderson, B. J. 2011. Plasticity of gray matter volume: the cellular and synaptic plasticity that underlies volumetric change. Dev Psychobiol, 53, 456-465.
[3]. Frank, E., Prien, R. F., Jarrett, R. B., Keller, M. B., Kupfer, D. J., Lavori, P. W., . . . Weissman, M. M. 1991. CONCEPTUALIZATION AND RATIONALE FOR CONSENSUS DEFINITIONS OF TERMS IN MAJOR DEPRESSIVE DISORDER - REMISSION, RECOVERY, RELAPSE, AND RECURRENCE. Archives of General Psychiatry, 48, 851-855.
[4]. Yoshimura, S., Okamoto, Y., Onoda, K., Matsunaga, M., Okada, G., Kunisato, Y., . . . Yamawaki, S. 2014. Cognitive behavioral therapy for depression changes medial prefrontal and ventral anterior cingulate cortex activity associated with self-referential processing. Soc Cogn Affect Neurosci, 9, 487-493.
[5]. Lai, C. H., & Wu, Y. T. 2014. Frontal-insula gray matter deficits in first-episode medication-naive patients with major depressive disorder. J Affect Disord, 160, 74-79.
[6]. Gold, P. W., Drevets, W. C., & Charney, D. S. 2002. New insights into the role of cortisol and the glucocorticoid receptor in severe depression. Biol Psychiatry, 52, 381-385.
Figures
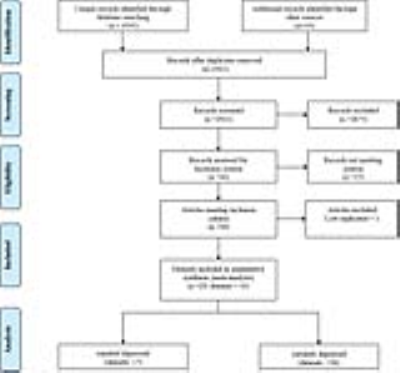
Figure 1. Literature search methods and results.
Abbreviations: MDD, major depression disorder.

Figure 2. Regional differences in grey matter volume in CMDD and RMDD compared with healthy controls by meta-analysis.
Abbreviation: ACC = anterior cingulate cortex; B = bilateral; CMDD = currently depressed patients; GR = gyrus rectus; IFG = inferior frontal gyrus; L = left; MCC = median cingulate cortex; R = right; RMDD = Remitted depressed patients; SFG = superior frontal gyrus.