5285
Does the presence of diffusely abnormal white matter in MS affect cognitive function?1Radiology, University of British Columbia, Vancouver, BC, Canada, 2Medicine, University of British Columbia, Vancouver, BC, Canada, 3UBC MS/MRI Research Group, University of British Columbia, Vancouver, BC, Canada, 4Neurology, University of Western Ontario, London, ON, Canada, 5Physics and Astronomy, University of British Columbia, Vancouver, BC, Canada, 6Pathology and Laboratory Medicine, University of British Columbia, Vancouver, BC, Canada, 7International Collaboration on Repair Discoveries, University of British Columbia, Vancouver, BC, Canada, University of British Columbia, Vancouver, BC, Canada
Synopsis
Multiple sclerosis (MS) subjects with diffusely abnormal white matter (DAWM) typically progress faster on physical disability scores. The impact of DAWM on cognitive measures is unknown. 50 MS participants had conventional MRI and cognitive tests of Trails Making Test, Working Memory, and Processing Speed. The presence of DAWM was not associated with worse cognitive performance. As DAWM is most commonly present in posterior regions of the brain, it may be that these cognitive tests were not sensitive to DAWM-associated pathology.
Introduction
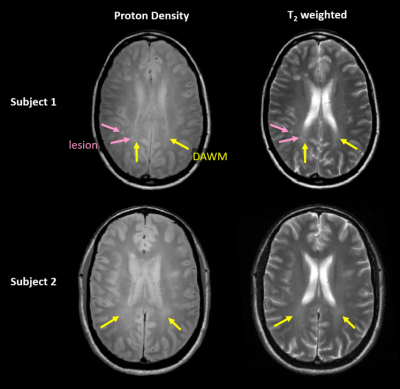
Multiple Sclerosis (MS) is a demyelinating disease of the central nervous system and is the most common neurological disorder in young adults, affecting 2.5 million people worldwide. In addition to many well-recognized physical symptoms1, up to 60% of MS patients experience cognitive deficits, which is now considered as one of the most disabling features of the disease2,3. Cognitive impairment has a significant impact on quality of life including daily living, socialization, and work4-7. Total lesion load and brain atrophy correlate with various aspects of cognitive dysfunction8-11. Another potential form of brain pathology which may impact cognitive function in MS is diffusely abnormal white matter (DAWM), which is found in ~25% of MS patients12,13. DAWM has poorly defined boundaries, with signal intensity higher than normal appearing white matter but not as high as lesions on proton density (PD) and T2-weighted MRI12,14. Histologically, DAWM shows blood-brain barrier breakdown and myelin and axonal loss15-18. DAWM may have clinical implications as patients with DAWM reach the same EDSS sooner than those without DAWM13,19. The impact of DAWM on cognitive dysfunction however is unknown.Objective
To examine the relationship between cognitive test scores and presence of DAWM as well as other clinical (EDSS, disease duration), MRI (lesion volume, normalized brain volume), and demographic variables (age, sex, years of education) in people with MS.Methods
Subjects: 50 MS patients (46 relapsing remitting, 4 secondary progressive; 37 females/13 males; mean age= 43.4yrs (range 22-60yrs); median EDSS = 2.0 (range 0-6.0); mean disease duration (DD) = 11.3yrs (range 0.33-36yrs); mean years of education = 14.7yrs (range 8-20yrs)).
MR Imaging: 3T conventional imaging with an 8-channel phase-array head coil (Philips Achieva, Best, Netherlands) included PD/T2 (TR/TE1/TE2=2800/8.4/80ms, voxel size=1x1x5mm3) and 3DT1 (MPRAGE, TR/TI=1800/817ms, voxel size=1x1x1mm3).
MRI data analysis: PD and T2 MRI scans were used to calculate lesion volume20, and determine the presence or absence of DAWM (Figure 1). Normalized brain volume (NBV) was calculated using the 3DT1 with a segmentation-based approach21.
Cognitive Testing: Tests included the Working Memory Index (WMI), Processing Speed Index (PSI) and Trails Making Test (TMTA and TMTB).
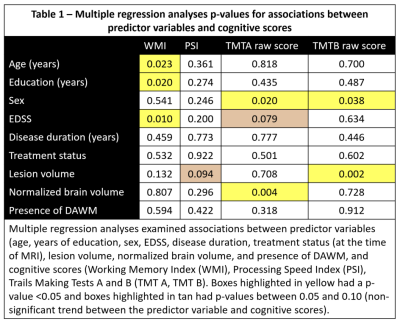
Statistical analysis: Multiple regression analysis (MRA) evaluated associations between age, years of education, sex, EDSS, DD, treatment status at the time of imaging, lesion volume, NBV and the presence or absence of DAWM on cognitive scores on the WMI, PSI and TMTA/TMTB.
Results
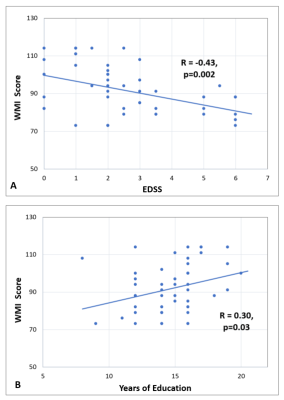
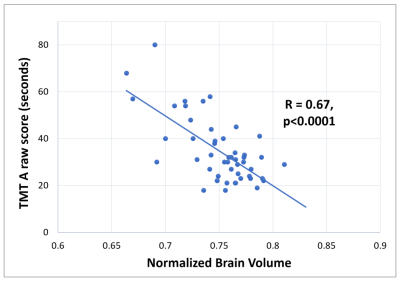
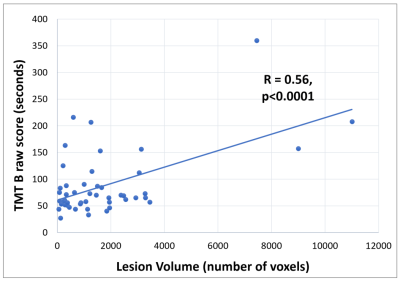
DAWM was found in 22/50 MS subjects. The presence of DAWM did not impact performance on any cognitive measure. WMI: Multiple regression analyses revealed that years of education (p=0.01) and age (p=0.02) were positively associated with WMI scores and EDSS (p=0.02) was negatively associated with WMI scores. PSI: There was a trend towards a negative association between lesion volume and PSI scores (p=0.09). TMT: TMTA performance was positively associated with female sex (p=0.02) and NBV (p=0.004) and there was a trend for a negative relationship between EDSS and TMTA performance (p=0.08). TMTB performance (a harder version of the TMTA task) was positively associated with female sex (p=0.04) and negatively associated with lesion volume (p=0.002). Table 1 summarizes multiple regression analysis p-values. Linear correlations between clinical/MRI measures and cognitive scores are shown in Figures 2,3,4.Conclusion
We found associations between cognitive scores
and years of education, age, EDSS, lesion volume, normalized brain volume and
sex but not the presence of DAWM. Although DAWM has been linked to faster
disability progression, as measured by EDSS, our results suggest DAWM may not
be linked to worse cognitive impairment. 44% of our subjects had DAWM, which is
higher than the rate of 25% previously reported at 1.5T12,13. One possibility is that at 3T, DAWM positive patients included those
with less severe abnormalities. Areas that were normal appearing at 1.5T might
have been identified as DAWM on 3T because of the improved resolution and
signal to noise at 3T. As DAWM is most
commonly found in the posterior regions of the brain, it may be that the cognitive
tests used were also not sensitive to DAWM-associated pathology. Further studies
using approaches which better assess posterior white matter brain function as
well as combining cognitive scores, rather than examining each independently, might
provide a more global reflection of cognitive impairment, and may be a more
comprehensive way to probe the cognitive impact of DAWM’s subtle and diffuse
damage. Acknowledgements
We would like to thank the
volunteers and their families and the wonderful technologists at the UBC MRI
Research Centre. This study is funded by the Multiple Sclerosis Society of
Canada.
References
1. Gelfand J. Multiple sclerosis: diagnosis, differential diagnosis, and clinical presentation. Handbook of Clinical Neurology: Elsevier; 2014:269-290.
2. Amato M, Zipoli V, Portaccio E. Multiple sclerosis-related cognitive changes: A review of cross-sectional and longitudinal studies. J. Neurol. Sci. 2006;245(1-2):41-46.
3. Pierson SH, Griffith N. Treatment of cognitive impairment in multiple sclerosis. Behav Neurol. 2006;17(1):53-67.
4. Bagert B, Camplair P, Bourdette D. Cognitive dysfunction in multiple sclerosis: natural history, pathophysiology and management. CNS Drugs. 2002;16(7):445-455.
5. Messinis L, Kosmidis MH, Lyros E, Papathanasopoulos P. Assessment and rehabilitation of cognitive impairment in multiple sclerosis. International Review of Psychiatry. 2010;22(1):22-34.
6. Rao SM, Leo GJ, Ellington L, Nauertz T, Bernardin L, Unverzagt F. Cognitive dysfunction in multiple sclerosis. II. Impact on employment and social functioning. Neurology. 1991;41(5):692-696.
7. Amato MP, Ponziani G, Siracusa G, Sorbi S. Cognitive dysfunction in early-onset multiple sclerosis: a reappraisal after 10 years. Arch. Neurol. 2001;58(10):1602-1606.
8. Sanfilipo MP, Benedict RH, Weinstock-Guttman B, Bakshi R. Gray and white matter brain atrophy and neuropsychological impairment in multiple sclerosis. Neurology. 2006;66(5):685-692.
9. Bomboi G, Ikonomidou VN, Pellegrini S, et al. Quality and Quantity of Diffuse and Focal White Matter Disease and Cognitive Disability of Patients with Multiple Sclerosis. J. Neuroimaging. 2010:E-pub ahead of print.
10. Benedict RH, Weinstock-Guttman B, Fishman I, Sharma J, Tjoa CW, Bakshi R. Prediction of neuropsychological impairment in multiple sclerosis: comparison of conventional magnetic resonance imaging measures of atrophy and lesion burden. Arch. Neurol. 2004;61(2):226-230.
11. Chiaravalloti N, Hillary F, Ricker J, et al. Cerebral activation patterns during working memory performance in multiple sclerosis using FMRI. J. Clin. Exp. Neuropsychol. 2005;27(1):33-54.
12. Zhao GJ, Li DKB, Cheng Y, et al. MRI dirty-appearing white matter in MS. Neurology. 2000;54 (suppl 3):A121.
13. Zhao G, Li DKB, Cheng Y, Paty DW, UBC MS/MRI Research Group, PRISMS Study Group. Possible prognostic significance of dirty-appearing white matter on MRI in multiple sclerosis. Mult. Scler. 2003;9(Suppl 1):S61.
14. West J, Aalto A, Tisell A, et al. Normal appearing and diffusely abnormal white matter in patients with multiple sclerosis assessed with quantitative MR. PLoS ONE. 2014;9(4):e95161.
15. Vos CM, Geurts JJ, Montagne L, et al. Blood-brain barrier alterations in both focal and diffuse abnormalities on postmortem MRI in multiple sclerosis. Neurobiol. Dis. 2005;20(3):953-960.
16. Moore GR, Laule C, Mackay A, et al. Dirty-appearing white matter in multiple sclerosis : Preliminary observations of myelin phospholipid and axonal loss. J. Neurol. 2008;255(11):1802-1811.
17. Seewann A, Vrenken H, van der Valk P, et al. Diffusely abnormal white matter in chronic multiple sclerosis: imaging and histopathologic analysis. Arch. Neurol. 2009;66(5):601-609.
18. Laule C, Vavasour IM, Leung E, et al. Pathological basis of diffusely abnormal white matter: insights from magnetic resonance imaging and histology. Mult. Scler. 2011;17(2):144-150.
19. Lycklama-a-Nijeholt GJ, van Walderveen MA, Castelijns JA, et al. Brain and spinal cord abnormalities in multiple sclerosis. Correlation between MRI parameters, clinical subtypes and symptoms. Brain. 1998;121 (Pt 4):687-697.
20. McAusland J, Tam RC, Wong E, Riddehough A, Li DKB. Optimizing the Use of Radiologist Seed Points for Improved Multiple Sclerosis Lesion Segmentation. IEEE Trans. Biomed. Eng. 2010;57(11):2689-2698.
21. Wicks E, Chiu JPC, Tang LYW, et al. Automatic Computation of Normalized Brain Volume on 3D T1-Weighted MRI Scans Without Registration to Standard Space. Paper presented at: International Society for Magnetic Resonance in Medicine 2015; Toronto, Canada.
Figures