5265
Diffusion tensor imaging in a rat model of brain stem ischemia reveals structural remodeling contralateral to the ischemic lesionLydia Wachsmuth1, Jens Minnerup2, Jan-Kolja Strecker2, Kai Diederich2, and Cornelius Faber1
1Clinical Radiology, Experimental NMR, University of Muenster, Muenster, Germany, 2Neurology, University of Muenster, Muenster, Germany
Synopsis
Ischemic stroke of the brain stem affects a considerable number of human patients. However, mechanisms of degeneration and recovery are not well understood and animal models of brain stem ischemia are rare compared to models of cortical stroke. Here we implemented a rat model of brain stem ischemia and applied diffusion tensor MR imaging as a noninvasive means to assess structural connectivity. Probabilistic mapping and histology indicate structural remodeling at the level of thalamus. These results add evidence for a potential compensatory mechanism for the observed partial recovery after brain stem stroke.
Introduction
Ischemic stroke of the brain stem affects a considerable number of human patients. However, animal models of brain stem ischemia are less common compared to models of cortical stroke. Mechanisms of degeneration and recovery cannot be simply inferred from studying hemispheric cortical lesions, because different brain areas exhibit varying potential of neurogenesis, and plasticity may differ in phylogenetically distinct regions. Here we used diffusion tensor imaging as a noninvasive means to assess structural connectivity in a rat model of brain stem ischemia.Methods
8 male Wistar rats (180-200 g) underwent induction of focal brain stem ischemia by photothrombosis. Under ketamine/xylazine anesthesia the base of the cranium was approached by blunt separation laterally from trachea and esophagus. A laser beam was targeted to the brain stem between midline and carotid canal. 3 min laser illumination at 560 nm through the skull was applied after i.v. injection of 1 mL Rose Bengal. Neurological deficits were assessed by behavioral testing (beam balance test, Rotarod, foot print test) and scoring over the course of the study. MRI under isoflurane anesthesia was performed at 9.4 T (Bruker Biospec) with a rat brain surface coil. We obtained sagittal and coronal 2D T2w RARE anatomical images pre, 2 weeks and 8 weeks after surgery. Diffusion tensor data were acquired pre and 8 weeks after surgery with an eight-segment EPI-DTI protocol (TR/TE 5000/30 ms) with 30 diffusion directions (b= 1000 s/mm², diffusion gradient duration = 5 ms, diffusion gradient separation = 11 ms) and five B0 images. Ischemic volumes were determined by threshold-based segmentation of the hyperintense areas in T2w MR images. We used dti_tool (University Hospital Freiburg, Germany, Dept. of Diagnostic Radiology, Medical Physics) for tensor calculation and probabilistic fibre tracking. Probability maps for two seed regions, left and right thalamus, were computed. The probability of connectivity between these seed regions was calculated by pixelwise multiplication of both maps1. Resulting maps with probability values above the threshold of 0.75 were overlaid with FA maps. ROI analysis was used to count the number of pixels comprising the connected area on the ipsi- and contralesional siteResults
T2w anatomical images (Figure 1) at two weeks after surgery revealed a brainstem infarct of 5.6 ± 3.5 µL within right brain stem in 6 of 8 rats. Neurological functions improved over time. At 8 weeks after surgery small hyperintense areas only remained in 4 of 6 ischemic rats. Probability maps of connectivity between seed regions in left and right thalamus revealed a central area with high probability values (>0.75) aligned with the medial longitudinal fissure between the right and left brain at Bregma -2 mm (Figure 2, yellow arrows). At baseline this area was symmetrically located across the midline. 8 weeks after surgery an increase of connected area on the contralesional site was found (Figure 3).Discussion and Conclusion
Diffusion tensor data provide information about structural connectivity. By multiplying probability maps based on different seed regions, one can extract pathways that show only those voxels where both maps are visiting and where the trajectories of the random walk analyses are opposed (indicating connecting rather than merging fibers). The higher number of connected voxels on the contralesional site at the level of thalamus agrees with the occurrence of midline crossing fibers in this area identified by anterograde cell tracing in an additional animal cohort of this study and may indicate axonal sprouting. We therefore conclude that DTI-based probabilistic mapping is able to resolve neuronal remodeling by axonal sprouting in the rat brain. Probabilistic mapping and histology add evidence for a potential compensatory mechanism for the observed partial recovery after brain stem stroke.Acknowledgements
No acknowledgement found.References
Kreher BW, Schnell S, Mader I, Il’yasov KA, Hennig J, Kiselev VG, Saur D, Connecting and merging fibers: Pathway extraction by combining Probability maps, Neuroimage 2008; 43(1):81-89)Figures
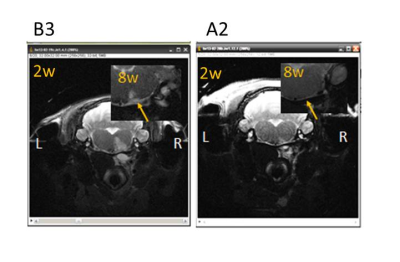
Figure 1: In T2w anatomical images (two exemplary rats)
the ischemic lesion appears as a hyperintense area within the right brain stem
at two weeks after surgery. At 8 weeks after surgery (insert) hyperintensities
are less apparent.
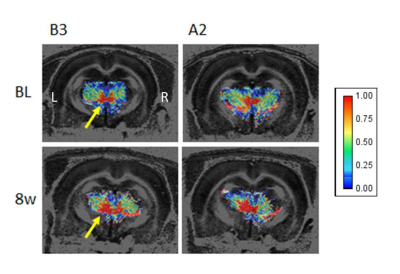
Figure 2: Probability maps of two rats (same as in
figure 1) at baseline and 8 weeks after surgery (cropped from a rectangular
area at the level of thalamus) overlaid on the respective FA maps. High
probability values are visible at the midline between left and right hemisphere
(yellow arrows). At 8 weeks after surgery the area with a high level of
connectivity is bigger contralateral to the lesion site.
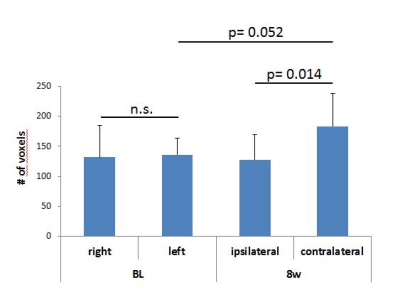
Figure 3: Quantitative analysis of the number of voxels
per hemisphere (threshold >0.75) visited by both probability maps as
indicated in figure 2. Mean values and SD are given. Data were tested for
normal distribution and compared with a paired t-test.