5263
Combining diffusion and perfusion weighted MRI measurements for disease and treatment monitoring in Multiple Sclerosis1Department of Imaging Sciences, University of Rochester Medical Center, Rochester, NY, United States, 2Department of Biostatistics and Computational Biology, University of Rochester Medical Center, Rochester, NY, United States, 3University of Rochester, Rochester, NY, United States, 4Department of Neurology, University of Rochester Medical Center, Rochester, NY, United States
Synopsis
In this large sample retrospective study of MS patients with different diagnoses and treatment regimens we investigated interactions between imaging metrics and age, MS phenotype, and types of treatment, and longitudinal changes associated with disease modifying treatments. We assessed WM injury using DTI metrics (FA, MD), and vascular changes (CBF and CBV) using perfusion DSC, in corpus callosum and in its cortical projections. We found significant correlations of perfusion with age, and DTI metrics with disease type and medication, suggesting that advanced neuroimaging methods such as DTI should become integrated into the clinical evaluation of MS patients for improved management.
Introduction: Due to its sensitivity, specificity and reproducibility MRI has a leading role in the assessment and management of multiple sclerosis (MS). The objective of this retrospective study was to investigate whether quantitative modalities that measure white matter (WM) integrity and cerebral blood flow (CBF) could provide additional insights in disease response to standard treatments. Specifically, our study evaluated retrospectively a large sample of MS patients with different diagnoses and treatment regimens, and examined interactions between imaging metrics and age, MS phenotype, and types of treatment, and if longitudinal changes in these metrics differ among disease modifying treatments. We assessed WM injury, as measured by diffusion tensor imaging (DTI) metrics (fractional anisotropy FA, mean diffusivity MD), and vascular changes (CBF and CBV) measured using perfusion dynamic susceptibility contrast (DSC) in corpus callosum (CC) and in its cortical projections. To our knowledge only one study correlated DTI and DSC metrics in CC of patients with relapsing-remitting MS (RRMS), and was limited by the small sample size1.
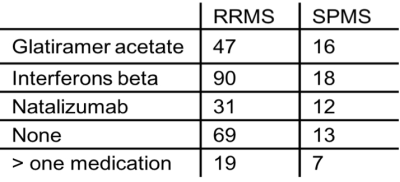
Methods: The study included 354 MS patients (264 F, 90 M) with MRI studies that included DSC and DTI. Most patients were diagnosed with RRMS (N=256, 361 scans), secondary progressive MS (SPMS) (N=66, 96 scans) and the rest had primary progressive MS or other demyelinating disorders such as neuromyelitis optica. Due to the larger numbers the study focused on patients with RRMS and SPMS. Treatment regimens are included in Table 1. Imaging data analysis: DTI data was processed using FSL2 software and included standard pre-processing. Probabilistic fiber tracking from corpus callosum (CC) to frontal, temporal, parietal and occipital lobes was performed and DTI metrics in these bundles were computed. Perfusion DSC data was processed using NordicIce software (NordicImagingLab, Bergen, Norway). Relative CBF, CBV and MTT maps were generated using tracer kinetic models applied to the first-pass data3 and corrected for extravascular contrast agent leakage4. Perfusion maps were registered with the DTI data and perfusion metrics were calculated in the ROIs described above. Statistical analysis: Linear mixed effects regression models were used to correlate imaging parameters, age, MS type, and types of treatment. For the longitudinal analysis, an additional random effect is used to account for serial correlation. Due to the large number of hypotheses being tested, Benjamini-Hochberg procedure was used to control the false discovery rate (FDR) at 0.05 level5.
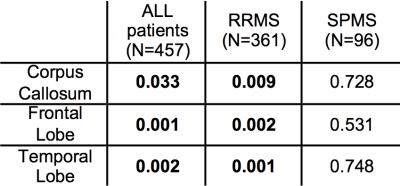
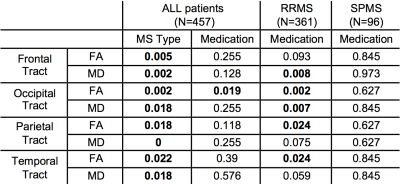
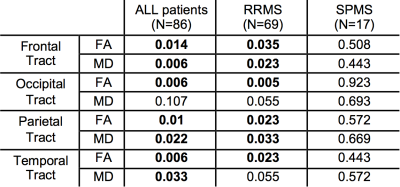
Results: There was a significant (p<10-5) age difference between the two patient groups (RRMS: mean age 44.32 years; SPMS mean age 50.83 years). The results of the linear regression analysis showing only significant correlations between imaging parameters (CBF, FA, MD) and other covariates are presented in Tables 2 and 3. Significant correlations were observed between perfusion metrics (CBF) and age, and between DTI metrics (FA and MD) and MS type. When the effect of treatment was evaluated on a subset of patients who had longitudinal data sets (69 RRMS, 17 SPMS) we found no significant effects of treatment on perfusion measures, and significant effects of Natalizumab on DTI metrics (Table4).
Conclusions: In this large sample size retrospective study of MS patients, we examined correlations between WM injury and vascular changes in corpus callosum and in its cortical projections and age, MS phenotype, and types of treatment. We found changes in perfusion associated with age as expected, but not with type of treatment. Changes in DTI metrics were significantly associated with disease type and medication. Further investigations of longitudinal changes revealed that only one treatment, Natalizumab, had an effect on WM integrity in RRMS, suggesting an increased protective effect of this drug when compared to other treatments. Despite the limitations of a retrospective study, the results strongly suggest that advanced neuroimaging analyses such as DTI should become integrated into the clinical evaluation of MS patients for best therapeutic management.
Acknowledgements
We would like to thank Dr. Sven Ekholm MD, Dr. Andrew Goodman MD, and Dr. Jessica Robb MD for help with identifying patients and imaging datasets, and their valuable insights with regard to study planning and interpretation.References
1. Saindane AM, Law M, Ge Y, Johnson G, Babb JS, Grossman RI. Correlation of diffusion tensor and dynamic perfusion MR imaging metrics in normal-appearing corpus callosum: support for primary hypoperfusion in multiple sclerosis. Am J Neurorad 2007;28:767-772.
2. Smith SM, Jenkinson M, Woolrich MW, et al. Advances in functional and structural MR image analysis and implementation as FSL. NeuroImage 2004;23 Suppl 1:S208-219.
3. Ostergaard L, Sorensen AG, Kwong KK, Weisskoff RM, Gyldensted C, Rosen BR. High resolution measurement of cerebral blood flow using intravascular tracer bolus passages. Part II: Experimental comparison and preliminary results. MRM 1996;36:726-736.
4. Boxerman JL, Schmainda KM, Weisskoff RM. Relative Cerebral Blood Maps Corrected for Contrast Agent Extravasation Significantly Correlate with Glioma Tumor Grade, Whereas Uncorrected Maps Do Not. Am J Neurorad 2006;27:859-867.
5. Benjamini, Y., and Y. Hochberg. 1995. “Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing.” J Royal Stat Soc: Series B 57: 289–300.
Figures