5194
3D nerve-sheath signal increased with inked rest-tissue rapid acquisition of relaxation enhancement imaging(3D SHINKEI) in traumatic brachial plexopathyShanshan Wang1, Guangbin Wang1, and Weibo Chen2
1Shandong medical imaging research institute, Jinan, China, 2Philips Healthcare,Shanghai,China, Shanghai, China
Synopsis
3D SHINKEI MRN with high spatial resolution ,is an extremely useful modality to image the traumatized brachial plexus and helps to accurately image the complete brachial plexus and localize as well as describe the lesions from the root still the terminal nerves.
Introduce
Traumatic brachial plexopathies is the most common nerve injury of the upper extremities .Nerve recovery is mainly determined by the interval between injury and treatment times , which in turn depends on early diagnosis1. However, the early determination of the degree of damage, the time of surgery, and the selection of surgical methods in traumatic brachial plexus injury patients still pose problems. Traditionally, brachial plexus injury has been evaluated using clinical history, physical examination, and neurophysiological testing. Neurophysiological tests and physical examination may not reveal the extent of the injury at the early stage and therefore may not supply the guideline of surgery time. Three-dimensional nerve-sheath signal increased with inked rest-tissue rapid acquisition of relaxation imaging (3D SHINKEI) is a new technique to suppress signals of blood vessels, muscles and fat tissue using improved motion-sensitized driven equilibrium (iMSDE) and spectral attenuated inversion recovery . With 3D SHINKEI, we can obtain images with high spatial resolution (0.98×0.97×2.0 mm 3 ) and evaluate the cervical ganglions and the brachial plexus from roots to branches. To the best of our knowledge, there has been no report using 3D SHINKEI to evaluate traumatic brachial plexopathies. Therefore, the purpose of this study was to evaluate the usefulness of 3D SHINKEI for traumatic brachial plexopathies.Methods
22 traumatic brachial plexopathies patients (18 male and 4 female, median age, 37 years; age range, 14–65years;) underwent 3D SHINKEI imaging of brachial plexus on a 3.0 T MR scanner (Achieva 3.0T TX; Philips Healthcare, the Netherlands) with a 16-channel neurovascular coil, TR/TE= 2400 ms /90 ms , FOV=220×310 mm, matrix=224×320, voxel size=0.98×0.97×2.0 mm 3 , b=10 s/mm 2 , iMSDE duration=50 ms. The source images were then reformatted by using maximum intensity projection (MIP) technique to optimize visualization of the brachial plexus. The contralateral side of brachial plexus was observed and evaluated as a normal reference. The imaging features of the contralateral brachial plexus were observed in all patients with the assistance of a qualified radiologist. All clearly visible brachial plexus ganglia,and extraspinal brachial plexus roots, trunks, branches and cords were counted. The MRI features of traumatic brachial plexopathies were observed and analyzed, followed by comparisons with intraoperative findings and EMG.Results
3D SHINKEI of brachial plexus has enabled good visualization of the small components of the brachial plexus. Visibility of the brachial plexus roots and ganglia were the highest(22/22), followed by that of trunks(21/22), branches(12/22) and cords(13/22). As for the 3D SHINKEI diagnosis of traumatic brachial plexopathies, the sensitivity, the specificity and the accuracy were respectively 97.6%, 96.3%, and 94.3%.Discussion
3D SHINKEI utilizes both spectral adiabatic inversion recovery type fat suppression and iMSDE. 3D iMSDE encompasses repeated opposite direction pulses for vascular signal suppression before the fat suppression and variable flip angle for T2W images are applied. The vessel signal-suppressed and fat-suppressed images have significant potential to produce high resolution and volumetric neurographic images2. The high resolution of images allows to localize as well as describe the lesions from the root still the terminal nerves of brachial plexus.Conclusion
3D SHINKEI MR neurography is an extremely useful modality to image the traumatized brachial plexus and helps to accurately image the complete brachial plexus and localize as well as describe the lesions from the root still the terminal nerves. It has a high correlation with surgical exploration and thus influences both surgical planning and outcome/prognosis.Acknowledgements
We thank Weibo Chen (Philips Healthcare) for providing technical assistance.References
1. Jivan, S., Kumar, N., Wiberg, M. & Kay, S. The influence of pre-surgical delay on functional outcome after reconstruction of brachial plexus injuries. J Plast Reconstr Aesthet Surg 2009,62(4), 472
2. Kasper JM, Wadhwa V, Scott KM, Rozen S, Xi Y, Chhabra A .SHINKEI-a novel 3D isotropic MR neurography technique: technical advantages over 3DIRTSE-based imaging. EurRadiol 2015,25:1672–1677.
Figures
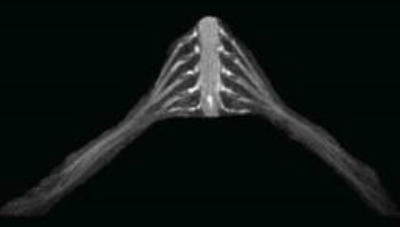
3D SHINKEI brachial plexus image with maximum-intensity projection (MIP) reconstruction and volume editing of a 26-year-old healthy male volunteer.
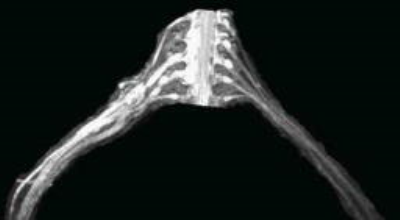
A 25-year-old man with history of road traffic accident one months back. 3D SHINKEI image shows disappearance of C6, neuroma formation and edema in roots,trunks,cords and branches of right brachial plexus.
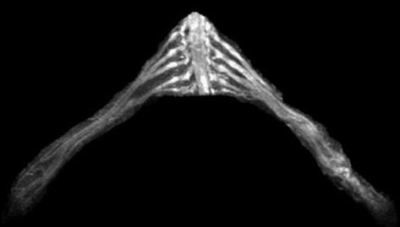
A 35-year-old man with history of stretch injury of left brachial plexus one weeks back. 3D SHINKEI image shows the tortuosity and edema in roots,trunks,cords and branches of left brachial plexus .